Complementary diagnostic and therapeutic approach of a rare inflammatory cloacogenic polyp—a case report
Highlight box
Key findings
• Narrow-band imaging (NBI) helps differentiate between neoplastic and non-neoplastic lesions. Newer endoscopic therapy, such as hybrid endoscopic submucosal dissection (ESD), is a feasible alternative to resect lesions arising from the anorectal region safely.
What is known and what is new?
• Inflammatory cloacogenic polyps are rare anorectal tumours that infrequently harbour the risk for malignancy.
• Characterisation with NBI serves as an added filter to better define the lesion and assist in performing targeted biopsies to improve diagnostic yield. Aside from surgical excision, endoscopic resection is equally safe and can be used to achieve good outcomes for surgically unfit patients.
What is the implication, and what should change now?
• The reliance on white-light imaging for endoscopic diagnosis may be inadequate. We highly encourage adopting NBI as a routine tool to complement detection and characterisation.
Introduction
Inflammatory cloacogenic polyps (ICPs) are a rare group of benign anorectal growths with comparable morphological and histological features to other pathologies seen in the full spectrum of ‘mucosal prolapse syndrome’ (1). Although the exact etiopathogenesis for ICP has yet to be defined, the current understanding is that they are likely to develop from recurrent mucosal ischemia and tissue regeneration. This proposed mechanism is analogous to other benign pathologies arising from separate anorectal regions, such as solitary rectal ulcer syndrome (SRUS), inflammatory ‘cap’ lesions and prolapsing mucosal polyps, thus, forming a continuum of disorders that derives its primary problem from disordered contractions, which leads to mucosal injury (2,3).
Patients with ICP tend to present mainly with complaints of per rectal bleeding and tenesmus. Other known associated symptoms include constipation, excessive straining, anal swelling, and itching, although up to 20% can be asymptomatic, for which the ICPs are an incidental finding during colonoscopies performed for other indications (4). Diagnosis of ICPs during colonoscopy may be challenging as it can mimic other rectal pathologies such as benign ulcers, haemorrhoids, adenomas, and cancers. However, with the advent of high-definition colonoscopes and the increasing use of narrow-band imaging (NBI), lesion characterisation can assist in real-time diagnosis to prevent under or overtreatment (5).
We recently encountered an elderly patient with a large anorectal ICP following a year’s complaint of haematochezia, in whom we performed an en-bloc endoscopic resection. Our case is unique as we are the second group to report the role of employing NBI in enhancing our diagnostic precision for ICPs and the first to describe the role of hybrid endoscopic submucosal dissection (ESD) as an option to the conventional ESD method for lesion excision. As opposed to the traditional ESD, which involves complete submucosal dissection, the hybrid ESD is a modified resection technique incorporating limited submucosal dissection followed by snare resection, thus, reducing procedural time without sacrificing patient and treatment outcomes. We present this case in accordance with the CARE reporting checklist (available at https://dmr.amegroups.org/article/view/10.21037/dmr-22-70/rc).
Case presentation
Our patient is an 88-year-old lady who presented with complaints of intermittent rectal bleeding for one year. She was initially diagnosed with haemorrhoidal bleeding and underwent rubber band ligation. The treatment was successful, and her symptoms disappeared until a month later, when she started redeveloping hematochezia. Aside from her main complaint of rectal bleeding, she denied experiencing altered bowel habits, diarrhoea, constipation, appetite or weight loss, pain or mucus discharge during defecation, perianal itching, faecal incontinence or prolapsing masses through her rectum during bowel movements. Her medical comorbidities included hypertension, dyslipidemia and nodal osteoarthritis, and her drug history was absent for antiplatelet and anticoagulation medications. Aside from consuming the occasional paracetamol for pain control, she denied taking traditional or herbal remedies. Clinical assessment was unremarkable except for the rectal examination that revealed a soft, flesh-like mass on the anterior rectal wall though there was no evidence of active bleeding. Biochemical investigations, including her coagulation profile, were unremarkable. The rectal bleeding had not affected her haemoglobin and iron levels.
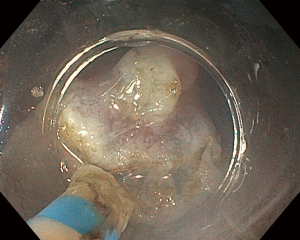
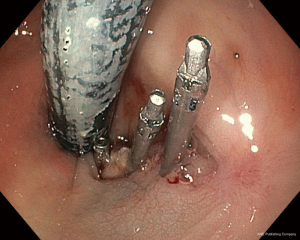
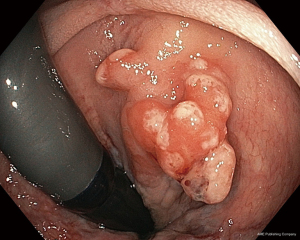
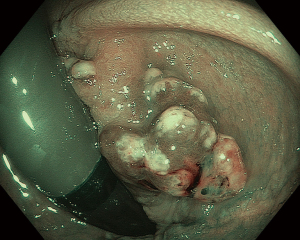
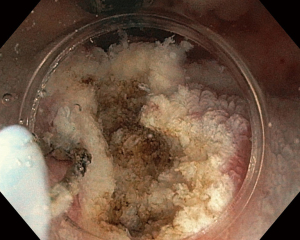
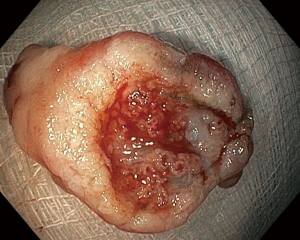
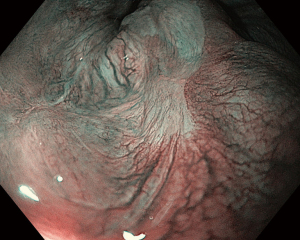
Index colonoscopy planned a week later demonstrated a large, 30 mm sessile polyp redder than the surrounding normal mucosa in the anterior wall of the anorectal junction. There were also multiple foci of fibrin deposition on the lesion’s surface, indicative of an inflammatory mass (Figure 1). Further characterisation with NBI did not reveal a dysplastic mucosal surface, as the overlying microsurface pit patterns were arranged regularly despite being swollen from ongoing inflammatory activity (Figure 2). The initial biopsy was unhelpful, revealing only non-specific inflammatory features, and following discussion with the patient, we obtained informed consent for endoscopic resection to acquire a larger specimen for diagnostic clarification. For our case, we selected the hybrid ESD technique, which began with a generous submucosal injection with a blend of indigo-carmine, gelafundin and adrenaline, followed by circumferential mucosal incision. Next, we performed a limited submucosal dissection using the DualKnife J electrosurgical knife (Olympus Medical System, Tokyo, Japan) (Figure 3). We then carefully place the 20 mm SnareMaster Oval (Olympus Medical System) snare around the dissected submucosal plane and complete the procedure with hot snaring using the ERBE VIO 200D (ERBE Electromedizin GmbH, Tubingen, Germany) electrosurgical unit (Figure 4). We tackled minor bleeding with the snare-tip soft coagulation technique and closed the defect with several haemoclips (Figure 5). Our patient went home the same day after a short observation in the recovery bay and experienced no immediate or delayed complications.
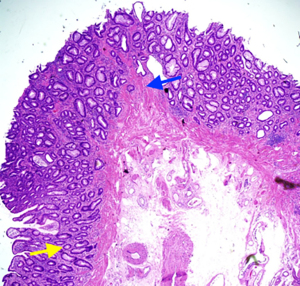
The resected specimen sent for pathological evaluation revealed key findings consistent with ICP: hyperplastic tubulovillous glands with elongated and irregular crypts with fibromuscular proliferation within the lamina propria (Figures 6,7). We repeated the colonoscopy three months later, for which the resected area had healed remarkably well with no endoscopic or histological recurrence (Figure 8).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
ICPs are a peculiar group of anorectal tumours that can take on the gross appearance of either a sessile, semi-pedunculated or pedunculated lesion while measuring an average of 10 to 50 mm in size (6). Morphologically, they are not too dissimilar from other benign and neoplastic pathologies and are known to coexist with other colorectal conditions such as internal haemorrhoids, diverticulosis, cancers, malabsorptive states, and Crohn’s disease (7). The connection between these concurrent disorders remains unclear, a knowledge gap that, if bridged, would assist in a better understanding of the aetiopathogenesis of ICP (8,9).
As a component by themselves, ICPs are generally benign owing to a vicious cycle of mucosal injury, reactive inflammation and subsequent reparative changes that lead to an overgrowth of fibromuscular tissue in the lamina propria (10). However, there have been instances where they reportedly undergo malignant transformation into cloacogenic carcinomas, prompting proposals for complete surgical excision or endoscopic resection, even in asymptomatic patients (9,10). Such potential risks of malignancy highlight the need for thorough detection during colonoscopy, including the much-debated benefit of performing endoscopic rectal retroflexion so as not to miss things. While some authorities advocated its usefulness in picking up more than 50% of neoplastic lesions missed in the antegrade view, recent prospective studies discovered that the role of retroflexion is limited to identifying other benign anorectal disorders, with no incremental yield in adenoma detection rates (11,12). This latter outcome sits very well with benign ICPs, as it would be impossible to inspect the anorectum by relying solely on antegrade views.
Separately, though recent improvements in colonoscope optics allow for easier differentiation between benign and malignant lesions, we must be mindful that white light imaging may be insufficient to arrive at a high-confidence diagnosis. And while there may be clues pointing toward the benign nature of polyps, such as the appearance of fibrin caps reminiscent of inflammatory polyps in our case, this can be misleading and cannot entirely exclude an underlying covert malignant component (13). In such instances, lesion characterisation by employing image-enhanced endoscopy (with or without magnification) like NBI to study the vessel and surface patterns of the polyp is a valuable, complementary tool to differentiate between neoplastic and non-neoplastic lesions (14). Furthermore, the additional capability of NBI to assist in targeted biopsy acquisition is equally beneficial to ensure greater diagnostic yield upon histopathological assessment.
Concerning management, the therapeutic pendulum has swung from surgery in favour of endoscopic resection in recent years, given the latter’s overall safety profile, lower morbidity and semi-invasiveness. After all, most ICPs are small to intermediate in size and require only conventional snare polypectomies, either through hot or cold snaring (15). However, larger polyps measuring more than 20 mm (with or without malignant transformation) are less common and, when encountered, would require advanced polypectomy techniques such as ESD to achieve en bloc resection (15,16). Currently, only one case report employed ESD in treating multiple ICPs with neoplastic transformation in an expert centre (17).
The lack of uptake in utilising ESD as a resection modality is mainly due to the lack of expertise, its’ time-consuming and the potential manoeuvrable difficulties in the anal canal, rendering the endoscope unstable. The development of hybrid ESD can address these technical issues by combining limited submucosal dissection and snare resection. During the dissection phase, the slightly splayed-open mucosa permits adequate visibility of the submucosal space, thus preventing snare slippage and optimising resection to minimise the risk of leaving behind tumour residues (18). Nevertheless, recent systematic reviews and meta-analyses still favour the traditional ESD approach to obtain clear resection margins though hybrid ESD remains a feasible alternative, especially when technical expertise is unavailable for conventional ESD and patients are unfit for surgery (19).
Our patient recovered without complications and was referred to a dietitian to advise on a high-fibre diet and increased fluid intake. The usual pharmacological agents of stool softeners and laxatives were also co-prescribed to minimise the risk of constipation and excessive straining in addressing the ICP’s pathogenesis (20). During subsequent follow-ups, there were no complaints of rectal bleeding, and a surveillance colonoscopy performed three months later demonstrated complete healing with no residual tumours. Although the current recommendation mandates ongoing endoscopic surveillance owing to the risk of recurrence, we need to balance these benefits against the inherent risk of procedural adverse events in an elderly patient with multiple comorbidities.
Conclusions
In closing, we wish to highlight that ICPs are rare anorectal tumours that infrequently harbour the risk for malignancy. With the advent of high-definition endoscopy and NBI, detection and characterisation in rectal retroflexion have an incremental gain in reducing the chance of missed lesions and allowing for differentiation between benign and neoplastic pathology (12). In terms of endoscopic resection, newer alternatives are emerging fast, and we believe that hybrid ESD has come to the fore to complement situations where a conventional ESD is unattainable. Nevertheless, these modern diagnostic and therapeutic strategies would require further research before implementation though we foresee this will be challenging owing to the rarity and under-recognition of ICP since its discovery in 1981.
Acknowledgments
We wish to express our sincere gratitude and appreciation by acknowledging our team of gastrointestinal nurses who assisted us and provided valuable insights and feedback during the colonoscopy. They are RN Norjanah Kamil, RN Julianie Julian, RN Rinah A/K Kijam, RN Rudy J. Perizin, and RN Roslina Yanting from Queen Elizabeth Hospital, Kota Kinabalu Sabah, Malaysia.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://dmr.amegroups.org/article/view/10.21037/dmr-22-70/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dmr.amegroups.org/article/view/10.21037/dmr-22-70/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lobert PF, Appelman HD. Inflammatory cloacogenic polyp. A unique inflammatory lesion of the anal transitional zone. Am J Surg Pathol 1981;5:761-6. [Crossref] [PubMed]
- Prakash N, Vyas SJ, Mohammed A, et al. Inflammatory Cloacogenic Polyp: A Rare Benign Colorectal Polyp. Cureus 2022;14:e22014. [Crossref] [PubMed]
- Monreal-Robles R, González-González JA, Benavides-Salgado DE, et al. Prolapsing mucosal polyp: A form of colonic polyp not to be forgotten. Rev Gastroenterol Mex (Engl Ed) 2019;84:407-9. [Crossref] [PubMed]
- López-Ramos CS, Rodríguez-Gómez S, Bailador-Andrés C, et al. Inflammatory cloacogenic polyp: a rare cause of lower gastrointestinal bleeding. Rev Esp Enferm Dig 2013;105:240-1. [Crossref] [PubMed]
- Saul SH. Inflammatory cloacogenic polyp: relationship to solitary rectal ulcer syndrome/mucosal prolapse and other bowel disorders. Hum Pathol 1987;18:1120-5. [Crossref] [PubMed]
- Levey JM, Banner B, Darrah J, et al. Inflammatory cloacogenic polyp: three cases and literature review. Am J Gastroenterol 1994;89:438-41. [PubMed]
- Tendler DA, Aboudola S, Zacks JF, et al. Prolapsing mucosal polyps: an underrecognized form of colonic polyp—a clinicopathological study of 15 cases. Am J Gastroenterol 2002;97:370-6. [Crossref] [PubMed]
- Parfitt JR, Shepherd NA. Polypoid mucosal prolapse complicating low rectal adenomas: beware the inflammatory cloacogenic polyp! Histopathology 2008;53:91-6. [Crossref] [PubMed]
- Hanson IM, Armstrong GR. Anal intraepithelial neoplasia in an inflammatory cloacogenic polyp. J Clin Pathol 1999;52:393-4. [Crossref] [PubMed]
- Marcos P, Eliseu L, Cunha MF, et al. Cloacogenic Polyps. ACG Case Rep J 2019;6:e00083. [Crossref] [PubMed]
- Varadarajulu S, Ramsey WH. Utility of retroflexion in lower gastrointestinal endoscopy. J Clin Gastroenterol 2001;32:235-7. [Crossref] [PubMed]
- Saad A, Rex DK. Routine rectal retroflexion during colonoscopy has a low yield for neoplasia. World J Gastroenterol 2008;14:6503-5. [Crossref] [PubMed]
- Pandit N, Yadav TN, Dahal M, et al. Inflammatory cap polyp of the sigmoid colon: a case report. J Med Case Rep 2021;15:306. [Crossref] [PubMed]
- Hayashi N, Tanaka S, Hewett DG, et al. Endoscopic prediction of deep submucosal invasive carcinoma: validation of the narrow-band imaging international colorectal endoscopic (NICE) classification. Gastrointest Endosc 2013;78:625-32. [Crossref] [PubMed]
- Kim YI, Joo JY, Yang HR. Inflammatory cloacogenic polyps in children: diagnostic yield of rectal retroflexion during colonoscopy. BMC Gastroenterol 2022;22:42. [Crossref] [PubMed]
- Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2017;49:270-97. [Crossref] [PubMed]
- Ochiai Y, Matsui A, Ito S, et al. Double Early Rectal Cancer Arising from Multiple Inflammatory Cloacogenic Polyps Resected by Endoscopic Submucosal Dissection. Intern Med 2021;60:533-7. [Crossref] [PubMed]
- Okamoto T, Ikeya T, Fukuda K. Hybrid endoscopic submucosal dissection for anal canal fibroma. VideoGIE 2022;7:154-7. [Crossref] [PubMed]
- McCarty TR, Bazarbashi AN, Thompson CC, et al. Hybrid endoscopic submucosal dissection (ESD) compared with conventional ESD for colorectal lesions: a systematic review and meta-analysis. Endoscopy 2021;53:1048-58. [Crossref] [PubMed]
- Shih CM, Tseng HH, Tu UC. Inflammatory cloacogenic polyp of anus: report of three cases. Zhonghua Yi Xue Za Zhi (Taipei) 1990;45:69-74. [PubMed]
Cite this article as: Chiam KH, Yong SM, Tan CC, Abdul Halim RA, Muthukaruppan R. Complementary diagnostic and therapeutic approach of a rare inflammatory cloacogenic polyp—a case report. Dig Med Res 2023;6:11.