
Ectopic esophageal sebaceous glands: a case report
Highlight box
Key findings
• Our study reports a rare disease of ectopic esophageal sebaceous glands, and summarized its endoscopic characteristics.
What is known and what is new?
• Ectopic esophageal sebaceous glands are really rare, and may be misdiagnosed with some other tumor disease. It is important to recognize its clinicopathological features.
• Our manuscript report here about a case of ectopic esophageal sebaceous glands, then discussed the possible pathogenesis.
What is the implication, and what should change now?
• Through understanding the pathologic features of this disease, more ectopic esophageal sebaceous glands should be recognized and learned.
Introduction
Sebaceous glands are widely distributed in the surface tissues of the human body. They are most abundant in the face and scalp, with a few glands in the chest and abdomen and with the fewest glands in the limbs. Sebaceous glands are closely related to hair follicles and form follicular sebaceous gland organs, most commonly in the face and scalp, but occasionally in abnormal areas. Ectopic sebaceous glands were first reported by Fordyce in 1896 as small yellow nodules in the mouth, lips, and rare genital mucosa, and were named Fordys spots (1). Ectopic sebaceous glands are mostly found in tissues and organs of ectodermal origin, including the lips, mouth, and palms; however ectodermal origin sebaceous glands are extremely rare in the esophagus. The earliest cases of esophageal sebaceous ectopicism were first reported by De La Pava in 1962 (2). Since 1978, all cases of the disease have been detected in living patients by endoscopy, but the disease is still very rare. We here report a case of ectopic esophageal sebaceous glands in accordance with the CARE reporting checklist (available at https://dmr.amegroups.com/article/view/10.21037/dmr-22-48/rc).
Case presentation
A 59-year-old female with a history of >10 years of thyroid nodules was admitted to the hospital, as she had been suffering from pain in front of the neck for >2 weeks. She had experienced subacute thyroiditis >30 years ago. At that time, she was treated with hormones and traditional Chinese medicine for about 1–2 years. Based on the patient’s thyroid color ultrasound that suggested inflammatory lesions, thyroid electroconvulsive therapy examination results, and history, a diagnosis of subacute thyroiditis was considered. Due to the patient’s complaint of recent frequent acid reflux, she underwent an upper endoscopy at The Seventh Affiliated Hospital of Sun Yat-sen University in February 2022.
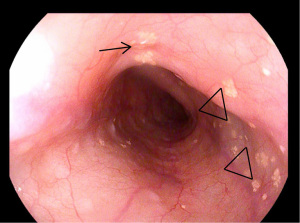
An esophagogastroduodenoscopy showed yellow-white granular hyperplasia on the mucosal surface, where the esophagus was about 25–30 cm from the incisor (see Figure 1). The mucosa of gastric antrum was hyperemic and red, with ≥6-spot flaky erosions. The following endoscopic diagnosis was made: (I) chronic superficial gastritis with erosions (grade III); (II) esophageal granular hyperplasia. The pathological examination revealed a yellowish, nearly round piece of esophageal mucosa, 0.1 cm in diameter, slightly irregular in shape, with a concave and convex surface that was soft to the touch. Under light microscopy, the examined tissue was observed to be covered with squamous epithelium. In the squamous epithelium, there were multiple focal lobular hyperplasia, lipid-containing, cytoplasmic foam sebaceous cells, which had a clear boundary with the squamous epithelium, accompanied by chronic inflammatory infiltration. The pathological diagnosis was ectopic esophageal sebaceous glands. After antigastritis treatment, the patient’s symptoms improved significantly. The patient continues to regularly visit the Endocrinology Department of our hospital so that her thyroid condition can be reviewed. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Ectopic esophageal sebaceous glands have only been observed rarely in clinical settings. In 1962, De La Pava examined 200 autopsy cases and was the first to report 4 cases of esophageal sebaceous adenosis (2). As upper gastrointestinal endoscopies have become more common, reports of esophageal sebaceous ectopia have increased, but most studies on the disease are reported on a case-by-case basis (3-5). In this case, the patient was an older adult woman who attended hospital for examination, complaining of gastrointestinal symptoms. The patient’s lesion was located in the middle and lower part of the esophagus, which is consistent with descriptions in the literature (6,7). Multiple yellowish-white papules or nodules were observed on the surface of the esophageal mucosa endoscopically. According to reports in the literature, the digestive endoscopic characteristics of this lesion are mostly multifocal, and a few are single focal (5).
Endoscopists need to understand the ectopic esophageal sebaceous glands to prevent misdiagnosis (8). As most primary hospitals in China have no pathology department, this endoscopic feature is of great significance in preventing the clinical misdiagnosis of lesions. The disease is relatively rare and needs to be differentiated from fungal infections, xanthelasma, and granular cell tumors. Magnifying endoscopy with narrow-band imaging may help to differentiate among these conditions (9).
Ectopic sebaceous glands may continue to perform their secretory functions, and to date, no associated symptoms have been reported. There is currently no evidence of an association between esophageal sebaceous ectopia and other diseases, such as gastroesophageal reflux and hyperlipidemia. In conclusion, ectopic esophageal sebaceous glands do not cause clinical symptoms, generally do not require treatment, and have a good prognosis provided there is a clear pathological diagnosis (10,11).
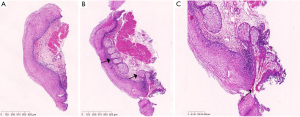
The histopathological examination results in this case revealed that the squamous intraepithelial morphology of the esophageal mucosa was generally normal, and there was only a small amount of inflammatory cell infiltration (see Figure 2A). After reviewing the gastrointestinal lens images, we decided to make a deep paraffin section. In this pathological section, well-differentiated sebaceous gland components were observed in the mucosal layer of the esophagus, and the sebaceous glands were observed to be partially wrapped around the scaly epithelium (see Figure 2B). In some cases, a small tubular opening may be microscopically observed in the center of the nodule as a small white protrusion that is an opening for a secretory catheter, and this characteristic is unique to the morphology of this lesion (4). This characteristic change was also observed in our case (see Figure 2C).
At present, there are 2 main hypotheses as to the origin of ectopic esophageal sebaceous glands (1). The first hypothesis is based on the theory of embryonic tissue dislocation, which holds that the disease is caused by an abnormal dislocation of sebaceous gland tissue during the development of the esophagus embryo. However, histoembryologists contend that the esophagus is an endoderm-derived tissue organ, while the sebaceous glands belong to the ectodermal source. Notably, no cases of esophageal sebaceous asteroid ectopia were found in a study examining the autopsies of 1,000 children (12). The second hypothesis is based on the metaplasia theory, which holds that the sebaceous glands are stimulated by factors such as gastric acid, chronic inflammation by the epithelium, or glandularization of the esophagus itself, which can be divided into 2 metaplastic sources.
One view is that sebaceous glands arise from submucosal glands inherent in the esophagus. It has been reported that the distribution and arrangement of sebaceous glands in the esophagus is very similar to the arrangement of submucosal glands, and the number of submucosal glands and ducts of the esophagus is comparable to the number of ectopic sebaceous glands (13). However, this conclusion has not been confirmed in many studies, and the submucosal glands of the esophagus are located in the submucosal layer. It is difficult to penetrate the mucosal muscle layer to the mucosal lamina, and the sebaceous glands are mostly located in the mucosal lamina. Another view is that the sebaceous glands are metaplasia from the scaly epithelium of the esophagus. Evidence supporting this view is that ectopic sebaceous glands are mostly located in the middle and lower esophagus, consistent with the lesion locations in the vast majority of reported cases, and the sebaceous glands are mostly located in the esophageal mucosa intrinsic layer, squamous subepithelial, and closely linked to the esophageal epithelium. This is consistent with the phenomenon observed in our reported case of a close relationship between the ectopic sebaceous glands and squamous epithelium.
Conclusions
In summary, we believe that it is very likely that the disease originates from the squamous epithelium of the esophagus, and there may be pluripotent stem cells with multiple differentiation potential in the squamous epithelial tissue are metamorphosed into sebaceous glands under the action of certain factors, with male hormones, for instance, potentially being one of the participating mechanisms. Male hormones play an important role in the development of human sebaceous glands. This also appears to explain why the disease occurs in adults and is more common in males than in females (10). However, the exact histological origin, etiology, and pathogenesis of the lesion have yet to be confirmed.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://dmr.amegroups.com/article/view/10.21037/dmr-22-48/rc
Peer Review File: Available at https://dmr.amegroups.com/article/view/10.21037/dmr-22-48/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dmr.amegroups.com/article/view/10.21037/dmr-22-48/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bhat RV, Ramaswamy RR, Yelagondahally LK. Ectopic sebaceous glands in the esophagus: a case report and review of literature. Saudi J Gastroenterol 2008;14:83-4. [Crossref] [PubMed]
- De La Pava S, Pickren JW. Ectopic sebaceous glands in the esophagus. Arch Pathol 1962;73:397-9. [PubMed]
- Jophlin LL, Hartley CP, Katzka DA. Ectopic Esophageal Sebaceous Glands. Clin Gastroenterol Hepatol 2022;20:e647. [Crossref] [PubMed]
- Le A, Amin M, Cappell MS. Case Report of a Proposed, Novel, Endoscopic "Whitehead Pimple" Sign of Ectopic Esophageal Sebaceous Glands Based on Their Mimicking the Dermatologic and Histopathologic Characteristics of Cutaneous Whitehead Pimples/Closed Comedones. Dig Dis Sci 2019;64:2049-53. [Crossref] [PubMed]
- Csanyi M, Arnaud M, Le Pessot F, et al. About 2 cases of ectopic sebaceous glands in esophagus: Endoscopic and histological correlations from biopsies and resected specimens. Ann Pathol 2016;36:134-8. [Crossref] [PubMed]
- Lee SH, Lee DJ, Kim KM, et al. Ectopic sebaceous glands in the oesophagus: a case report and review of literature. Scott Med J 2014;59:e1-5. [Crossref] [PubMed]
- Peixoto A, Rodrigues S, Silva M, et al. Esophageal ectopic sebaceous glands. Acta Gastroenterol Belg 2017;80:321. [PubMed]
- Humes RJ, Sadowksi BW, Long JO, et al. An Odd Place for Acne: Ectopic Esophageal Sebaceous Glands. ACG Case Rep J 2020;7:e00465. [Crossref] [PubMed]
- Jeon MS, Kim GH, Jeong DY, et al. Magnifying Endoscopy for Esophageal Ectopic Sebaceous Glands. Clin Endosc 2018;51:495-7. [Crossref] [PubMed]
- Park A, Lee JH, Park A, et al. Prevalence rate and clinical characteristics of esophageal ectopic sebaceous glands in asymptomatic health screen examinees. Dis Esophagus 2017;30:1-5. [Crossref] [PubMed]
- Fukuchi M, Tsukagoshi R, Sakurai S, et al. Ectopic Sebaceous Glands in the Esophagus: Endoscopic Findings over Three Years. Case Rep Gastroenterol 2012;6:217-22. [Crossref] [PubMed]
- Rector LE, Connerley M. Aberrant mucosa in the esophagus in infants and children. Arch Pathol 1941;31:295-94.
- Hoshika K, Inoue S, Mizuno M, et al. Endoscopic detection of ectopic multiple minute sebaceous glands in the esophagus. Report of a case and review of the literature. Dig Dis Sci 1995;40:287-90. [Crossref] [PubMed]
(English Language Editors: L. Huleatt and J. Gray)
Cite this article as: Zhang T, Huang J, Wang B, Zhang J, Liao D, Zhu J, Xue L. Ectopic esophageal sebaceous glands: a case report. Dig Med Res 2023;6:19.


