A case of ectopic bronchogenic cyst in the stomach and a review of relevant literature
Overview
Bronchogenic cysts are cystic masses caused by abnormal congenital development of the respiratory system. According to location of this disease, bronchogenic cysts are divided into the intrapulmonary type, mediastinal type, and ectopic type. When cysts are small, there may be no clinical manifestation; when cysts enlarge or are combined with infection, they can cause compression symptoms or infection symptoms in surrounding tissues. This article reports the diagnosis and treatment of one young woman with ectopic bronchogenic cysts in the stomach and a review of the relevant literature.
Data
The patient was admitted to our hospital after 8 d of repeated fever. The patient did not have chest pain or abdominal pain, did not have urinary tract irritation symptoms, and had normal urination and defecation. The patient had a medical history of rhinitis and cholecystitis for more than 10 y and denied a medical history of tuberculosis or genetic diseases. A physical examination of abdomen did not show obvious masses.
Auxiliary examinations
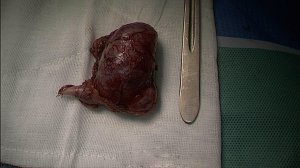
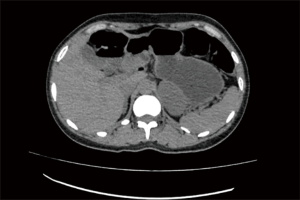
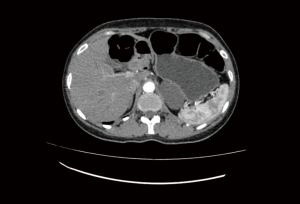
Computed tomography (CT) showed an oval-shaped, low-density mass on the left side area of the left upper abdominal spine. The boundary of the mass was clear, the mass was closely associated with the posterior wall of the stomach and the left adrenal gland locally, the left adrenal gland was compressed, the front and rear sides of the mass were adjacent to the gastric wall, and the size was approximately 5.5 cm ×3.5 cm. The CT value was approximately 27 HU, and enhanced scanning showed mild enhancement. There was no observed enlargement of the lymph nodes around the mass and in the retroperitoneum (Figures 1-4). Gastroscopic examination showed normal gastric mucosa, and there was no mass in the gastric cavity.
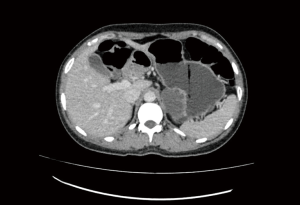

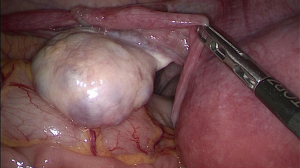
Multidisciplinary discussion after the patient was admitted considered a high possibility of a benign mass; therefore, laparoscopic resection of the mass in the posterior wall of the stomach was selected. The surgery was successful. Intraoperative incision of the gastrocolic ligament showed that the mass was located above the pancreatic tail (Figure 5). The tumor was completely removed (Figure 6).
Postoperative pathology (gastric mass)
The tumor body was located in the serosal layer and muscular layer of the gastric wall and was cystic. The cystic wall was composed of thin smooth muscle bundles and adipose tissues. The inner wall of the cavity was covered with multiple layers of bronchial ciliated columnar epithelium. The cells had no abnormal shapes, and there were scattered mucinous and serous glands in several small foci and focal lymphocytic infiltration in the cystic wall. The lesion was consistent with a benign cyst, specifically, a bronchogenic cyst.
Discussion
Etiology
Bronchogenic cysts are rarely encountered in clinical practice. The incidence is not high, and it is a rare disease. Bronchogenic cysts are a type of residual embryonic cystic glands that result from bronchial dysfunction during embryonic development (1). During embryonic development, the airway epithelium is separated from the tracheobronchial tree and develops to other locations from the bronchus. The bronchial cyst lining has respiratory epithelia composed of goblet cells filled with mucin and ciliated pseudostratified columnar epithelia. They are predominantly located in the mediastinum and lung tissues (2). Cysts that occur outside the lungs are called ectopic bronchogenic cysts.
Bronchogenic cysts can occur at any location in the body. They can occur in the retroperitoneum, subcutaneous tissue, lower neck, brain parenchyma, paranasal sinus, and spinal canal and can also occur in the esophagus, pericardium, and mediastinum (3). Generally, they are located near the midline in areas such as the trunk, head and neck; there are no reports of bronchogenic cysts in locations such as the four limbs, which might be associated with the embryonic development of the foregut. The case in this report was a young woman. She was at an age consistent with the age of predilection in the reported literature (4). Because the connection between epithelial cells is very tight, the degree of expansion of the cyst is limited. Thus, the growth rate of ectopic bronchogenic cysts is usually slow, the disease onset is insidious, the disease develops primarily after the patient reaches adulthood, and clinical symptoms are not typical. Therefore, the majority of cases are discovered during physical examinations (3).
Diagnosis
Bronchogenic cysts usually do not have clinical symptoms. For example, this case sought treatment due to repeated fever, and the mass in the abdominal cavity was discovered after repeated examinations to determine the cause of the fever. Bronchogenic cysts do not have specific clinical symptoms and physical signs. The mass in this case was from the abdominal cavity and was derived from the stomach. It was adjacent to the left adrenal gland, and the size of the mass was 5.5 cm × 3.5 cm. The cyst did not cause temporary gastrointestinal symptoms in this patient. When the cyst is deposited in the mucous membrane and enlarges and compresses surrounding organs and tissues, patients might experience upper abdominal discomfort, such as nausea, vomiting, abdominal pain, low back pain, and urinary tract infection (5).
The discovery and diagnosis of bronchogenic cysts rely on imaging. Cysts will not have enhancement or will have mild enhancement on CT enhancement scans, and there is no strong blood supply to the tumors. CT plain scans show low-density shadows with a clear boundary. After other types of tumors are excluded, the possibility of bronchogenic cysts should be considered. Changes in the CT values of the lesion can confirm whether it is cystic or solid. Half of all cysts show soft tissue densities due to thick secreted substances; such cysts are easily misdiagnosed as solid masses. Bronchogenic cysts usually have dark brown mucus inside. The protein concentration is high, and the cystic wall is very thick, which cause an increase in the CT density. In addition, there are differences among typical cysts (6). In a few cases, CT values are negative. Those cases should be distinguished from teratomas. Calcification can occur inside cysts, and a very small number of cases show high densities due to calcification (7,8).
Magnetic resonance imaging (MRI) can help with the diagnosis and differential diagnosis of bronchogenic cysts. On MRI, the majority of bronchogenic cysts are a single mass. They are usually round or oval, the boundaries are clear, and the sizes are different. According to the literature reports, the smallest diameter is less than 1 cm, and the largest diameter is less than 20 cm (9). Because the pressure in the gap is low, tumor growth along the gap is consistent with the growth pattern. When the mass grows larger, compression symptoms will occur. The wall of these cysts is thin and is not visible on MRI or appears as a thin line. T1 shows isointense signals, and T2 shows hypointense signals. CT cannot distinguish the capsule wall, and small dots of calcification may even be observed. If the cyst contains clear cystic fluid, the cyst will have long T1 and long T2 signals indicating water density on MRI. If the cystic fluid has a consistency similar to coffee or jelly, it will present a high density shadow on CT images close to the soft tissue density. Doubly high signals in MRI indicate that the protein content is high and that this type of cysts is more likely. The presence of mixed signals indicates bleeding and infection. Because of inflammatory cell infiltration and swelling, a compound infection will thicken the wall. Similar to the CT enhancement findings, enhancement changes are also not present on enhanced MRI (10).
CT and MRI are conducive to the localization of bronchogenic cysts and the determination of the compression degree of surrounding tissues. However, the final diagnosis of bronchogenic cysts still relies on pathology. In pathological paraffin sections, the discovery of single-layer or pseudostratified columnar epithelia, smooth muscle, elastic fibers, cartilage, or other tissue containing mucous glands can allow an immunohistochemistry diagnosis without auxiliary methods. In this case, multiple layers of bronchial ciliated columnar epithelium were discovered in pathological sections, the cells were resected, and there were several small foci with mucus, serous glands, and focal lymphocytic infiltration in the cystic wall. Therefore, the findings in this case were consistent with bronchogenic cysts.
Bronchogenic cysts are benign lesions. There is currently no literature report of malignant cases in China. Surgical resection is the only method for treating this disease. The cystic wall should also be completely resected to the fullest extent possible during surgery. If the cyst is ruptured, it generally will not cause recurrence or metastasis. There is currently no case of recurrence and metastasis in the literature reports. However, surgery for ectopic bronchogenic cysts presents a high degree of difficulty. Bronchogenic cysts in the mediastinum require thoracotomy, and the resulting trauma is considerable. If surgical resection is not performed, the continuous enlargement of cysts can cause compression symptoms. The risk of thoracotomy is high. With the development of endoscopic techniques, cysts in mediastinum and the abdominal cavity can be completely resected under a laparoscope, which greatly reduces patient trauma. The cyst in this case was located in the posterior wall of the stomach and was completely resected under a laparoscope. The difficulty of surgery for cysts in the retroperitoneum is high, and the associated surgical risk is high. Postoperative recovery is slow. Resection under a laparoscope is usually difficult, and open abdominal resection is usually required; this is the reason for the high surgical risk and the slow postoperative recovery.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2019.09.04). YH serves as the Editor-in-Chief of Digestive Medicine Research. CZ serves as an unpaid Associate Editor-in-Chief of Digestive Medicine Research. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Guo Z, Li G, Zhang Y. Two cases of retroperitoneal bronchogenic cyst and literature review. Chin J Urol 2012;33:608-10.
- Ribet ME, Copin MC, Gosselin B. Bronchogenic cysts of the mediastinum J Thorac Cardiovasc Surg 1995;109:1003-10. [J]. [Crossref] [PubMed]
- Chongyi S, Meng Y, Dejun Y, et al. Lumbar intradural extramedullary bronchiogenic cyst. Eur Surg Res 2008;40:26-8. [Crossref] [PubMed]
- Sumiyoshi K, Shiminzu S, Enjoji M, et al. Bronchogenic cyst in abdomen. Virchows Arch 1985;408:93. (pathol Anat). [Crossref] [PubMed]
- Li L, Liu J, Luo Y, et al. Clinical and ultrasonographic findings of ectopic bronchogenic cyst of the abdomen are easily misdiagnosed. Chinese Journal of Medical Imaging 2018;26:438-41.
- Cai Y, Guo Z, Cai Q, et al. Bronchogenic cysts in retroperitoneal region. Abdom Imaging 2013;38:211-4. [Crossref] [PubMed]
- McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, et al. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology 2000;217:441-6. [Crossref] [PubMed]
- Yang DM, Jung DH, Kim H, et al. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics 2004;24:1353-65. [Crossref] [PubMed]
- Qin M, Liu S, Huang JB. CT diagnostic value of ectopic bronchial cyst. CT Theory and Applications 2016;25:587-92.
- Yang B CT. Journal of Clinical Radiology 2012;31:591-4.
Cite this article as: Li J, Liu Y, Deng Q, Jiang J, Chen H, Zhang C, He Y. A case of ectopic bronchogenic cyst in the stomach and a review of relevant literature. Dig Med Res 2019;2:29.