Boerhaave syndrome complicated by undiagnosed gastroesophageal junction outlet obstruction: a case report
Introduction
Boerhaave syndrome is a condition carrying high morbidity and mortality, necessitating emergency intervention. Along with appropriate resuscitation and drainage, accepted definitive therapy aims for either open transpleural primary closure, placement of an endoluminal covered stent, or sometimes a combination of both strategies. Only in very rare cases does a rupture occur exclusively within the abdomen, without violation of either pleural space. Occasionally, a patient’s premorbid esophageal anatomy presents special challenges—such as stricture, malignancy, or other structural complexity—that requires alternative approaches to addressing both immediate and long-term recovery.
We present a case in which the patient’s vague history and current imaging suggest undiagnosed gastroesophageal junction outlet obstruction (GEJOO), possibly achalasia, which in large part contributed to his rupture. Also unusual is the isolation of the spontaneous tear to the abdomen. In this case we detail the integration of strategies to repair his injury, protect the repair, and help prevent recurrence of dysphagia or rupture. We present the following case in accordance with the CARE reporting checklist (available at https://dmr.amegroups.com/article/view/10.21037/dmr-22-61/rc).
Case presentation
A 64-year-old, relatively healthy nonsmoker male presented with 6 hours of chest pressure after having choked on chicken meat and then retched extensively. He reported two prior episodes of dysphagia in his lifetime, including an episode of food bolus 5 months earlier, at which time he underwent an esophagogastroduodenoscopy (EGD) that revealed an extensive mucosal tear at 30–35 cm from the incisors. There was no stricture identified at that time; the patient was discharged on oral Protonix and had no follow-up.
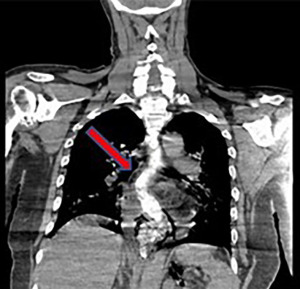
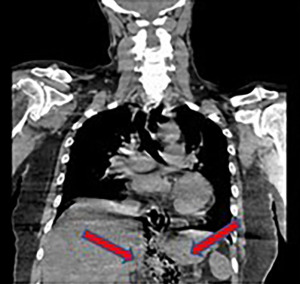
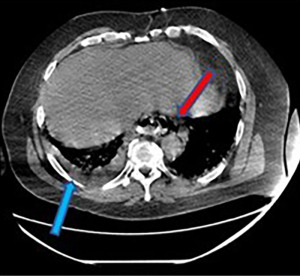
During the present admission, he was tachycardic, in visible distress with pallor and diaphoresis, with a distended and tender abdomen, without peritonitis. Computed tomography (CT) esophagram revealed a very tortuous and dilated esophagus with tight narrowing at the gastroesophageal (GE) junction, contrast spillage in the lower right epigastrium, and extensive free air in the retroperitoneum and abdominal space. There were also bilateral small pleural effusions without evidence of intrapleural contrast extravasation (see Figures 1-3). Abnormal lab values demonstrated leukocytosis to 19.4 K/µL and creatinine elevated to 1.56 mg/dL.
After fluid resuscitation and antibiotics, the surgical team made plans for immediate, definitive surgical intervention.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Operation
In the operating room, the decision was made to approach the distal esophageal leak via laparotomy. After safe entry, a nasogastric tube was guided into the stomach. The hiatus was then gently exposed, revealing a 4-cm longitudinal transmural defect at the right posterolateral aspect just 2 cm proximal to the GE junction. No other abnormalities were seen at the hiatus, therefore approximately 8 to 10 cm of mobilization was undertaken into the mediastinum. The tissue at the esophageal injury was friable, and mucosa unable to be fully exposed based on body habitus and difficult exposure, so a classical two-layer closure was not possible. We did, however, place full-thickness interrupted silk sutures followed by another running silk layer, with the nasogastric tube as a guard against stricture.
We then planned for fundoplication for optimal coverage of the repair, as well as to complement a contralateral myotomy, which would aim to help prevent recurrence of narrowing at the GE junction and adequately treat GEJOO as his presumptive diagnosis. Short gastric vessels were divided with LigaSure device (Medtronic, Minneapolis, MN, USA); the fundus was found to be very generous and estimated to be able to accommodate a loose 360-degree wrap. We then undertook a myotomy on the esophagus contralateral to the injury, extending approximately 6 cm proximal to the GE junction, and 4 cm distal to the GE junction onto the gastric cardia. Nissen fundoplication was then performed, using three double-pledgeted Ethibond sutures (Ethicon, Cincinnati, OH, USA), with the upper two sutures incorporating intact esophageal wall. Per-oral bougie was not used based on tortuosity of the esophagus. When completed, the wrap extended approximately 4 cm, and covered both the injury repair and myotomy sites. Gastric feeding tube was then placed via standard Stamm technique, and a large drain was left within the lesser sac. The patient tolerated the procedure well and was extubated within 6 hours.
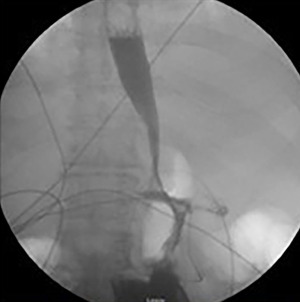
During his recovery period, the patient was kept nil per os (NPO). The gastrostomy tube was initially used for decompression, then on postoperative day (POD) 2 he began receiving tube feeds. On POD 5, a water-soluble contrast study was performed (see Figure 4), demonstrating nearly normal esophageal morphology and transit, healed leak site, with prompt contrast passage via lower esophageal sphincter (LES) and pylorus. The retroperitoneal drain, from which very little thin drainage was captured after surgery, was discontinued. The patient was then started on a clear liquid diet and quickly advanced to a post-Nissen regimen. He was discharged to home on POD nine and was found in clinic to be recovering very well at POD 22, at which time his gastrostomy tube was removed. The patient experienced no adverse events during the hospital course or post-op follow-up.
Discussion
Esophageal rupture most commonly occurs due to iatrogenic causes, while about 15% of cases involve Boerhaave type injury induced by forceful vomiting. This phenomenon was first described by Dutch physician Herman Boerhaave (circa 1724) (1) and carries a mortality rate of between 10% and 40% in collected series (2). This type of rupture, isolated to the abdomen, is exceedingly uncommon; in one of the largest worldwide meta-analyses of 75 studies, involving 2,971 patients over 12 years, only 77 patients were identified to have had abdominal involvement (3). Meanwhile, we find a case describing achalasia-related injury, in which an elderly female suffered an intrathoracic rupture, was treated with multiple stents, and succumbed to her condition within 1 month (4). Another published case describes Boerhaave syndrome secondary to benign GEJOO. In the case report they describe an elderly female who presented with a gastric volvulus as the cause of the esophageal rupture. The patient underwent surgical drainage and irrigation of the mediastinum and pleural cavities, followed by a gastrostomy to fix and decompress the stomach. The patient was discharged after an uneventful hospital course (5).
Generally accepted principles of successful therapy for esophageal rupture include timely recognition, thorough resuscitation, and earliest treatment according to the individual clinical details of this very heterogeneous condition (3). Primary repair and stent placement show similar survival rates, while patients whose acuity mandates control measure such as t-tube, have a much higher mortality. Patients with esophageal cancer, or who require esophagectomy, fare very poorly (3).
GEJOO, such as achalasia, displays an incidence of approximately 1 per million per year, and is characterized by the Chicago Classification (6). This class of disorders, in general, involves abnormalities of both excitatory and inhibitory motor neurons, interfering with esophageal body muscle contraction as well as relaxation of the LES (6,7). High resolution manometry is currently the standard of care for diagnosis, classification, and determination of recommended treatment and prognosis. Our patient, in extremis, was unable to undergo formal esophageal testing, therefore the strong clinical clues—food bolus episodes in the past, “bird’s beak” type of LES narrowing and esophageal dilation and tortuosity upon presentation—were utilized to plan for immediate surgical remedy that would also accommodate for longer term recovery. Strong data show between 81% and 100% success rate of myotomy and fundoplication for all types of GEJOO (8), and our patient’s postop studies show no GE junction stenosis and resolution of the esophageal dilation and tortuosity, so this appears to have been the right procedure for the patient. In the longer term, our patient will undergo follow-up manometric studies, as well as surveillance imaging and endoscopy.
Conclusions
Herein we have presented a patient with a life-threatening, spontaneous type of esophageal tear, with the complicating feature of a previously underestimated GEJOO. Prompt recognition of his acute injury, along with identification of his esophageal anatomy, allowed for a technically feasible repair, with very smooth, early and midterm recovery.
GEJOO should be considered when a patient presents with a rupture of the esophagus and abnormal esophageal anatomy on imaging. This will allow for potential incorporation of myotomy and fundoplication in the surgical repair.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://dmr.amegroups.com/article/view/10.21037/dmr-22-61/rc
Peer Review File: Available at https://dmr.amegroups.com/article/view/10.21037/dmr-22-61/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dmr.amegroups.com/article/view/10.21037/dmr-22-61/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Turner AR, Turner SD. Boerhaave Syndrome. 2021. In: StatPearls. Treasure Island: StatPearls Publishing, 2022.
- Chirica M, Kelly MD, Siboni S, et al. Esophageal emergencies: WSES guidelines. World J Emerg Surg 2019;14:26. [Crossref] [PubMed]
- Biancari F, D'Andrea V, Paone R, et al. Current treatment and outcome of esophageal perforations in adults: systematic review and meta-analysis of 75 studies. World J Surg 2013;37:1051-9. [Crossref] [PubMed]
- James TW, Brimhall BB, Baron TH. Use of multiple covered metal esophageal stents for treatment of Boerhaave syndrome in achalasia. VideoGIE 2019;4:549-50. [Crossref] [PubMed]
- Saito S, Hosoya Y, Kurashina K, et al. Boerhaave's syndrome in a patient with an upside down stomach: A case report. Int J Surg Case Rep 2016;19:51-4. [Crossref] [PubMed]
- Ihara E, Muta K, Fukaura K, et al. Diagnosis and Treatment Strategy of Achalasia Subtypes and Esophagogastric Junction Outflow Obstruction Based on High-Resolution Manometry. Digestion 2017;95:29-35. [Crossref] [PubMed]
- Cassella RR, Ellis FH Jr, Brown AL Jr. Fine-structure changes in achalasia of the esophagus. I. vagus nerves. Am J Pathol 1965;46:279-88. [PubMed]
- Francis DL, Katzka DA. Achalasia: update on the disease and its treatment. Gastroenterology 2010;139:369-74. [Crossref] [PubMed]
Cite this article as: Anderson RP, Budde J, Stevens T. Boerhaave syndrome complicated by undiagnosed gastroesophageal junction outlet obstruction: a case report. Dig Med Res 2023;6:5.