
The effects of exercise prehabilitation in upper gastrointestinal oncology patients undergoing surgical resection: a systematic review
Introduction
Upper gastrointestinal (UGI) cancers; including oesophageal, gastric, hepatic, pancreatic and biliary, were responsible for >25% of all cancer associated deaths worldwide in 2020 (1). Despite recent advances in patient perioperative care, the 5-year survival rates in this group are consistently amongst the worst of all tumour types: oesophageal is 20%, gastric is 32%, pancreatic is 10%, liver is 20% and biliary is 10% (2). The stubbornly low 5-year survival rate is mainly attributable to the advanced stages of the disease at diagnosis, as these cancers are often aggressive with symptoms occurring late and in a more elderly population (3). The consequence of which is that by diagnosis <50% of all patients in this group will have resectable disease, this drops to as low as 15% in pancreatic cancer patients (3). To date, systematic reviews and meta-analyses investigating the impact of prehabilitation (PH) on patient outcomes in GI cancer have always included colorectal carcinoma as a sub-group. This group generally gets diagnosed earlier through surveillance screening resulting in a lower disease burden at time of surgery with a significantly improved prognosis (63% 5-year-survival) compared to the UGI cohort. This systematic review was therefore designed to exclude this group of patients to generate a better understanding on how feasible it is to conduct exercise PH programs within the more functionally frail UGI cohort.
For UGI patients that do have a resectable disease, a combined surgical and oncological approach including neoadjuvant chemotherapy (NAC) and adjuvant chemo(radio)therapies is essential for treatment with curative intent (4). However, even with recent surgical advancements, these operations are highly complex and are associated with a significant degree of postoperative morbidity (5). neoadjuvant therapies are often poorly tolerated and can result in reduced patient functional capacity leading up to their procedure (6). This coupled with an elderly cohort and the inevitable disease-related decline in physiological status including sarcopenia, malnourishment and frailty (7), mean this group has a significantly higher rate of postoperative complications when compared to the rest of the surgical population (8).
This is of particular concern in this cohort as the best chance of overall and disease-free survival occurs when patients can complete their whole postoperative course of chemo(radio)therapy (9). Unfortunately, recent studies have shown that only 50–55% of gastric cancer patients will successfully return to their intended oncological treatment (RIOT) (10,11). The inability to RIOT has also been linked to a reduced disease-free survival in liver (9) and pancreatic (12) cancer patients. The most common reasons for failure to RIOT are poor preoperative patient functional status and a high incidence of major postoperative complications (9,10). This has prompted a growing body of research to investigate whether taking measures to improve a patients’ preoperative functional capacity can lead to a reduction their postoperative morbidity, allowing for a higher RIOT rate and ultimately prolonged disease-free survival (13).
PH is “the practice of enhancing a patient’s functional capacity before surgery with the aim of improving post-operative outcomes” (14). PH programs are a relatively new concept in perioperative care, they aim to tap into the unique window of opportunity that arises in the preoperative period to encourage patients to make long-lasting changes to their health and lifestyle. Initially PH programs were predominantly exercise focused (15), but more recently they have started to evolve into multi-modal interventions including respiratory, nutritional and psychological components (16,17). Whilst there is now evidence that some of these programs can improve preoperative functional capacity, the optimal strategy is still unknown (17,18). Should programs include aerobic or resistance muscle training, should they be multimodal or unimodal, should exercise be home or hospital based? Different disease processes are likely to benefit from different types of intervention depending on the length of time to surgery, preoperative morbidity and baseline function (14,16,19).
This systematic review has been designed to look particularly at the exercise component of PH programs in UGI cancer patients with the aim of ascertaining what the best and most pragmatic approach for this cohort is. Intuitively the optimal PH program is likely to be multimodal (20), but given the many unanswered questions still surrounding the various exercise interventions that have been trialled, it is important to gain a better understanding of this particular aspect of PH so we can better analyse the other components in due course.
Aims
- Primary outcome: to assess the feasibility of conducting an exercise based PH program in UGI oncology patients prior to undergoing surgical resection by evaluating patient compliance alongside improvements in overall functional capacity.
- Secondary outcome: to evaluate the effectiveness of these PH programs on post-operative outcomes, including length of stay, complications, and patient quality of life (QoL) assessments.
This systematic review was reported in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) reporting checklist (21) (available at https://dmr.amegroups.com/article/view/10.21037/dmr-21-84/rc).
Methods
The study protocol was submitted to the Brighton and Sussex Medical School Dissertation Committee for review on 8th June 2020 with full approval granted with no amendments required on the 2nd of July 2020. The review protocol can be made available on request.
A systematic literature search was carried out using the following databases: Medline, Embase, PubMed and CINAHL utilising the NICE Healthcare Databases Advanced Search (HDAS) tool (22). The first search was carried out on the 21st June 2020 with a second on 10th May 2021. There were no date restrictions for the included publications and results were limited to English language publications.
Six different search terms were used separately across the four databases aiming to capture PH studies across the UGI cancer spectrum: “(upper abdominal surgery OR upper gastrointestinal surgery) OR (oesophagectomy OR oesophageal cancer) OR (gastrectomy OR gastric cancer) OR (liver resection OR liver cancer) OR (pancreatectomy OR pancreaticoduodenectomy OR pancreatic cancer) OR (hepatobiliary cancer) AND (prehabilitation OR exercise)”. Following the database search, a further search of the grey literature was also conducted. This search primarily utilised the “google scholar” global search engine along with a review of citations found in editorials, other systematic reviews, guidelines and protocols. Once through the eligibility screening process, these results were then added to the final included studies from the database search.
All abstracts were screened for eligibility by EMT. Inclusion criteria included patients >18 years undergoing UGI cancer surgery following an exercise based PH program. Multi-modal PH programs were included, but they had to have an exercise component. All studies had to include an objective measure of functional capacity pre- and post-exercise PH to assess adherence and efficacy of the exercise program. This was the main marker used to assess feasibility of the individual programs. If there was any ambiguity about including a particular study then this would be discussed with MM and CJ for a consensus opinion. No extra information was required of the authors from any of the full text articles reviewed.
The following data was manually extracted from each eligible article by EMT; patient demographics, study characteristics including the number of patients involved, study design, duration and cancer diagnosis, composition of the PH programs (exercise ± nutrition ± psychological), method of delivery, compliance and supervision of the PH programs, any preoperative changes in functional capacity following the introduction of these programs and any effects these PH programs had on post-operative outcomes and patient perceived QoL scores.
To ensure the conclusions drawn from this systematic review were robust and accurate, it was important that each study used within the review was assessed for quality and the potential risk of bias. One way to significantly reduce the risk of bias would be to only use randomised controlled trials (RCTs), however, due to the paucity of data currently available for PH programs in UGI cancer patients, non-randomised trials were also included provide a more complete understanding of what research has been conducted so far. To ensure the quality of these non-randomised trials, the Cochrane Risk of Bias in Non-randomised Studies-1 (ROBINS-1) tool was used (23). The risk of bias in the RCTs was assessed using the Risk of Bias-2 (ROB-2) tool from the Cochrane group (24). The risk of bias assessment was conducted by EMT and CJ, no studies were excluded due to an unacceptably high risk of bias.
On careful consideration of the studies eligible for inclusion in this review it was not considered appropriate to conduct a meta-analysis. The clinical variability within the studies in terms of program duration, design and functional capacity assessments did not easily lend themselves to whole group or sub-group statistical analysis. A meta-analysis in this case would at best be meaningless and at worst obscure genuine results/outcomes.
Results
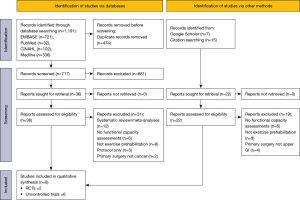
Following the initial database search, 1,191 publications were identified, duplicates were manually removed and screened for inclusion, 36 articles were left for eligibility screening. From the grey literature search, 22 articles were identified for eligibility screening. The full text articles were then obtained for all 58 articles, with 8 studies left completing the eligibility criteria. Figure 1 outlines the flow diagram of the complete study identification process for this review.
Of the 8 studies included within this review, 2 were RCTs and 6 were observational prospective cohort studies, one of which contained matched pair analysis.
Risk of bias
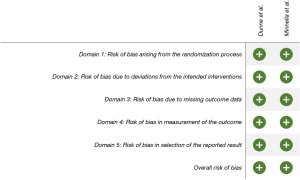
The overall risk of bias for both RCTs was low risk, see Figure 2.
The risk of bias for the cohort studies was assessed using the ROBINS-1 assessment tool, see Figure 3. As expected, there were areas in all the studies that were at a moderate risk of bias, the most common being the risk of confounding bias or bias in the measurement of outcomes.

Bias due to confounding was more prevalent in Mikami et al. (25), Ngo-Huang et al. (26) and Valkenet et al. (27). One reason for confounding bias is the self-selecting nature of patients for the PH programs, generally patients who are more motivated, live closer to the hospital or less frail will be more inclined to sign up to such programs. Valkenet et al. (27) looked at the baseline characteristics of those choosing not to participate found participants had significantly less severe disease than non-participants (P=0.04). The self-selecting process has a lower bias risk in Nakajima et al. (28) as they used matched pair analysis, Halliday et al. (29) as only one patient in 67 opted out and Yamamoto et al. (30), as all those deemed eligible were enrolled.
Bias in the measurement of outcomes was moderate across 4 of the studies (26,28-30). This was predominantly due to the self-reporting nature of the home-based programs which could be significantly over-estimated by some patients resulting in a falsely elevated level of adherence and compliance.
Study characteristics
Of the 8 studies included for review, 3 had a patient control group, the 2 RCTs (31,32) and the matched pair analysis from Nakajima et al. (28). The other 5 were observational studies (25-27,29,30). Two studies looked specifically at oesophageal cancer patients (29,32), two at pancreatic cancer patients (25,26), one at patients with liver metastatic disease (31), one at gastric cancers (30), one with hepato-pancreato-biliary (HPB) cancers (28) and one with a mix of all GI cancers (27). There was a total of 402 patients in the PH groups across the studies, 208 of which underwent NAC. Table 1 further outlines the characteristics of the studies included in this review.
Table 1
| Study | Design | Type of surgery | No. of patients in PH group | No. of patients in CN group | No. of patients having NAC |
|---|---|---|---|---|---|
| Dunne et al. (31) | RCT | Liver resection for colorectal metastasis | 20 | 17 | 22 (12 in PH, 10 in CN) |
| Minnella et al. (32) | RCT | Oesophageal cancer | 26 | 25 | 35 (20 in PH, 15 in CN) |
| Mikami et al. (25) | Cohort | Pancreatic cancer | 26 | 0 | 22 |
| Ngo-Huang et al. (26) | Cohort | Pancreatic cancer | 50 | 0 | 50 |
| Nakajima et al. (28) | Cohort | Open abdominal surgery for HPB cancers | 76 | 76 | 0 |
| Halliday et al. (29) | Cohort | Oesophageal cancer | 67 | 0 | 60 |
| Yamamoto et al. (30) | Cohort | Gastric cancer | 22 | 0 | 0 |
| Valkenet et al. (27) | Cohort | GI cancer (pancreatic, liver, intestinal, gastric or oesophageal) | 115 | 0 | 44 |
PH, prehabilitation; CN, control group; NAC, neoadjuvant chemotherapy; RCT, randomised controlled trial; HPB, hepato-pancreato-biliary; GI, gastrointestinal.
Composition of PH programs
Table 2 shows an overview of the PH programs in each of the studies. All of the studies were required to have an exercise component as part of the eligibility criteria, 3 studies had a nutritional element (28,30,32) and one a psychological element (29). The duration of the programs varied significantly with Ngo-Huang et al. (26) and Halliday et al. (29) choosing to start their programs at the time of diagnosis which enabled them to commence the program prior to patients undergoing NAC treatment resulting in 16-week duration. The shortest programs were 1–2 weeks, one of which was hospital based (25), the other home (30).
Table 2
| Study | Design | Components of the PH program | Mean duration (weeks) | Type of exercise | ||
|---|---|---|---|---|---|---|
| Exercise | Nutrition | Psychological | ||||
| Dunne et al. (31) | RCT | × | 4 | HIIT on bike | ||
| Minnella et al. (32) | RCT | × | × | 5 | Mix aerobic and resistance | |
| Mikami et al. (25) | Cohort | × | 1–2 | Mix aerobic and resistance | ||
| Ngo-Huang et al. (26) | Cohort | × | × | 16 | Mix aerobic and resistance | |
| Nakajima et al. (28) | Cohort | × | × | 4–5 | Walking and resistance | |
| Halliday et al. (29) | Cohort | × | × | 16 | Mix aerobic and resistance | |
| Yamamoto et al. (30) | Feasibility | × | × | 2 | Walking and resistance | |
| Valkenet et al. (27) | Feasibility | × | 4–5 | Mix aerobic and resistance | ||
×, component was included in the program. PH, prehabilitation; RCT, randomised controlled trial; HIIT, high intensity interval training.
Type of exercise intervention
There was a significant amount of heterogenicity between the type and intensity of exercise involved. All the studies except for Dunne et al. (31) incorporated an element of resistance training as well as aerobic.
Two looked specifically at home-based walking interventions alongside resistance training. Yamamoto et al. (30) aimed for a daily step count of >7,500 whereas Nakajima et al. (28) only required 30 minutes 3× per week. However, the mean duration of the program was 2× longer in the Nakajima et al. cohort (28).
Three of the other studies also used a home-based mixed exercise program of aerobic and resistance training but in these the aerobic exercises involved walking, cycling or jogging (26,29,32). Minnella et al. (32) and Ngo-Huang et al. (26) both required 60 minutes/week of aerobic exercise with 1 and 2 resistance training sessions/week respectively. Halliday et al. (29) aimed for 150 minutes of aerobic exercise/week with an individualised program for resistance training.
Mikami et al. (25), whose program had a significantly shorter mean duration than almost all the other studies, set up a hospital-based program involving daily 50-minute aerobic sessions encompassing walking and cycling alongside added resistance training. Valkenet et al. (27) was the only study to use a mixture of home-based and hospital-based programs. This program consisted of 2× week aerobic and resistance training as part of a group session followed by a further 30 minutes 5× per week moderate-vigorous exercise at home.
Supervision and compliance
Method of exercise delivery, supervision and compliance can be seen in Table 3. The highest levels of compliance can be seen in the hospital-based supervised programs (25,31). Ngo-Huang et al. (26) also had relatively high compliance, especially considering the duration of this program was 16 weeks. This was the only study to use an objective measurement of physical activity for a home-based program, patients were encouraged to wear an accelerometer for 2 consecutive weeks at the mid-point of each phase of treatment. Yamamoto et al. (30) had the lowest compliance levels of all the studies, this may partly be due to their elderly sarcopenic cohort coupled with the daily exercise requirement.
Table 3
| Study | Design | Mean duration (weeks) | Method of delivery | Supervision | Compliance |
|---|---|---|---|---|---|
| Dunne et al. (31) | RCT | 4 | Hospital-based, 12× interval bike sessions | Y | 95% |
| Minnella et al. (32) | RCT | 5 | Home-based with 3× week aerobic and 1× week resistance training + individualised nutritionist plan with supplements | N | 63% |
| Mikami et al. (25) | Cohort | 1–2 | Hospital based, daily aerobic and resistance | Y | 100% |
| Ngo-Huang et al. (26) | Cohort | 16 | Home-based, 60 mins/week aerobic and 60 mins/week resistance training | N | 84% |
| Nakajima et al. (28) | Cohort | 4–5 | Home-based, 3× weekly walking and resistance training + leucine-rich amino acid daily supplementation | N | Unknown |
| Halliday et al. (29) | Cohort | 16 | Home-based, 150 mins/week aerobic + resistance training. Increasing intensity over time. Motivational sessions with nurse | N | 56% during NAC; 65% after NAC; 85% no NAC |
| Yamamoto et al. (30) | Feasibility | 2 | Home-based, daily walking and resistance training + individualised dietician plan | N | 50% |
| Valkenet et al. (27) | Feasibility | 4–5 | Mix home and hospital-based. Hospital: 2× weekly aerobic and resistance training. Home: inspiratory muscle training + 5× weekly aerobic | Partly | Hospital-based: 82%; home-based: unknown |
Y, yes; N, no. PH, prehabilitation; RCT, randomised controlled trial; NAC, neoadjuvant chemotherapy.
Halliday et al. (29) assessed compliance levels in patients who underwent NAC, both during and after their treatment, as well as those with no NAC. Unsurprisingly the level of compliance with their exercise program improved once NAC treatment had ended, but compliance levels never reached that of the no NAC sub-group.
Outcomes of the PH programs
Table 4 shows an overview of the outcomes from the studies PH programs, including changes in preoperative functional capacity, post-operative complications, and patient QoL surveys.
Table 4
| Study | Design | Functional capacity outcome measures | Preoperative changes in functional capacity | Post-operative complications | Health related QoL |
|---|---|---|---|---|---|
| Dunne et al. (31) | RCT | VO2 max + AT | SI in AT by 1.5 mL/kg/min, and VO2 max by 2 mL/kg/min | No difference | SI: in both physical and mental health |
| Minnella et al. (32) | RCT | 6MWD | SI in 6MWD—improved in 62% in PH vs. 4% in CN | No difference | Not assessed |
| Mikami et al. (25) | Cohort | 6MWD + VO2 max + AT | SI in VO2 max across all ages and sexes. SI in AT in males and <75 years old only. SI in 6MWD across all ages and sexes | No control | Not assessed |
| Ngo-Huang et al. (26) | Cohort | 6MWD | SI in 6MWD | No control | Lower scores in patients with baseline frailty and reduced compliance with PH |
| Nakajima et al. (28) | Cohort | 6MWD | SI in 6MWD in both males and females | SI in post-op length of stay (median 23 vs. 30 days, P=0.045) | Not assessed |
| Halliday et al. (29) | Cohort | VO2 max and O2 pulse | VO2 max and O2 pulse were maintained during NAC with then a SI in the period following NAC prior to surgery | Amount of weekly PA sig associated with the risk of pneumonia | Not assessed |
| Yamamoto et al. (30) | Feasibility | 4-m gait speed | Not significant | No control | Not assessed |
| Valkenet et al. (27) | Feasibility | VO2 max | Not significant | No control | No improvement |
PH, prehabilitation; QoL, quality of life; RCT, randomised controlled trial; VO2 max, maximal oxygen consumption achieved during the test; AT, anaerobic threshold; SI, significant improvement; 6MWD, 6-minute walk distance; CN, control group; O2 pulse, indirect measurement of stroke volume; PA, physical activity.
Changes in preoperative functional capacity
Three studies used the 6-minute walk distance (6MWD) as their functional capacity assessment (26,28,32), three used maximal oxygen consumption achieved during test (VO2 max) ± anaerobic threshold (AT) (27,29,31), one study used both of these functional measures (25) and one looked at 4-m gait speed (30).
All the studies looking at 6MWD showed significant improvements following their PH programs. Three of these were home-based programs of 5–16 weeks duration (26,28,32), one was hospital based with 1–2 weeks duration (25), indicating that even with limited time it is feasible to meaningfully improve preoperative functional capacity in this cohort.
Of the studies looking at VO2 max, only one out of four did not show any significant improvement, Valkenet et al. (27). Yamamoto et al. (30) also showed no significant improvement in 4-m gait speed following their 2-week home-based program.
Postoperative complications
There was no difference in the incidence of post-operative complications in either of the RCTs. Nakajima et al. (28) used matched pair analysis to compare their current PH cohort with historic data which showed a significant decrease in length of stay in the PH group by an average of 7 days.
Halliday et al. (29) collected data on the incidence of post-operative pneumonia in their patient cohort. The data showed that the average weekly physical activity over the whole 16-week program significantly associated with the risk of pneumonia. The higher the average weekly activity, the lower the incidence of post-operative pneumonia.
QoL outcomes
Most studies did not collect any patient centred outcome data. Three looked at patient QoL outcome data (26,27,31). Valkenet et al. (27) used the 36-item short form survey (SF-36) and the EORTC QLQ-30 (European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire), Dunne et al. (31) used the SF-36 survey and Ngo-Huang et al. (26) used the FACT-Hep (Functional Assessment of Cancer Therapy-Hepatobiliary) questionnaire. Only Dunne et al. (31) found a meaningful increase in patient QoL.
Discussion
This systematic review shows it is feasible to conduct preoperative exercise-based PH programs in UGI cancer patients and that these programs can significantly improve their functional capacity prior to surgery.
Functional capacity outcome measurements
Despite a significant degree of heterogenicity across the studies in terms of duration, composition and mode of administration, six of the eight studies reviewed reported a significant improvement in functional capacity using either the 6MWD (25,26,28,32) or cardiopulmonary testing to ascertain VO2 max ± AT (25,29,31). Of the four studies using VO2 max ± AT, two used a standard cardiopulmonary exercise testing (CPET) approach of maximal exercise testing on a cycle ergometer to provide direct measurements of CPET-derived variables including VO2 max and AT (25,31). This technique is now well established as an objective measure of functional capacity and validated as a risk prediction tool for postoperative morbidity and mortality across a wide variety of major surgical procedures (33,34). The other two studies used submaximal exercise testing to provide indirect VO2 max measurements, one via the Chester Step Test (29) and the other utilising the Astrand nomogram (27). The ability of these studies to accurately predict VO2 max has recently been evaluated via direct comparison to CPET (35). The Chester Step Test was found to be valid for predicting mean changes of VO2 max in a group of patients, but that individual predictions were liable to considerable error (35). As this systematic review is focused on mean group improvements in VO2 max following the implementation of a PH program, this method of functional capacity assessment is appropriate for use in this context. The validity of the Astrand test was less conclusive (35,36). The test requires patients to cycle for 5–6 minutes with heart rates of 120–170 bpm for the Astrand nomogram to predict a VO2 max value. Patients with limited endurance or on beta blockers found it difficult to reach and maintain these heart rates, causing a high drop-out rate for this test in the evaluation study (35). Valkenet et al. (27) only have Astrand VO2 max results for 38% of their PH patients, from which they were unable to observe any significant improvement following their PH program. The write up for this study was done a few years after it was conducted, and the authors are unable to account for the 62% of missing data. Steps have been taken to minimise the effects of this data gap by using a mixed-models analysis to try to provide an unbiased estimate of the missing data. Given the high volume of missing data and the potentially high drop-out rates using the Astrand method of testing, it would seem prudent to use alternative validated measurement methods for functional capacity testing in the future, such as CPET or the 6MWD.
The 6MWD was utilised by four studies (25,26,28,32) and is a validated measurement tool for functional capacity assessment (37). A significant change of 20m deviation from baseline was used across the studies in keeping with previous definitions (38). The 6MWD has been shown to correlate well to CPET-derived variables in both cardiac (39) and non-cardiac (40) surgery, there is also evidence that 6MWD may be useful in predicting postoperative outcomes including complications (41) and length of stay (42), but the distance thresholds required to define the higher-risk group are yet to be determined. All of the studies using the 6MWD as a measurement tool showed a significant improvement in their patient cohorts following their PH programs.
Yamamoto et al. (30) used 4-m gait speed as their measure of functional improvement. Attempts to validate this technique against the 6MWD have shown that whilst there is some correlation between the two, 4-m gait speed has a reduced correlation in comparison to the 6MWD with age, lung capacity and muscle strength and therefore its ability to accurately assess functional performance is uncertain (43). Yamamoto et al. (30) found no significant difference in the 4-m gait speed following their PH program.
Feasibility of PH programs during NAC
The feasibility of PH programs in the UGI cancer cohort is highly dependent on these patients being able to adhere to exercise interventions whilst undergoing or having just completed a course of NAC. Six of the studies in this review had patients undergoing NAC (25-27,29,31,32), two of which conducted 16-week programs capturing data on patient adherence both during and after NAC treatment (26,29). Both these studies found a significant improvement in functional capacity tests by the end of their programs. Halliday et al. (29) also tested patients in the middle of their PH program following NAC completion, at this point they found no improvement in functional capacity but more significantly, no deterioration. The effects of chemotherapy on patient fitness have been well documented, there is often a substantial fall from baseline in these patients that struggles to improve back up to baseline prior to surgery (44,45). Therefore, the maintenance of functional capacity during NAC in Halliday et al. (29) followed by a significant improvement from baseline in the weeks prior to surgery is very encouraging. Compliance to the PH program in Halliday et al. (29) also differed significantly depending on where patients were in their treatment cycle. Compliance was at its lowest at 56% in patients undergoing NAC, rising to 65% when treatment was completed, those that never required NAC had a much higher compliance rate of 85%. The compliance rate in the other 16-week study, Ngo-Huang et al. (26), was up at 84% with every patient in this study undergoing NAC. Both of these PH programs were home-based and relied at least partly on patient self-reporting for compliance (Ngo-Huang also intermittently used accelerometers), and these results show that not only are patients undergoing NAC able to adhere to a PH program, but by attenuating the usual functional decline, they also stand to make significant improvements to their preoperative functional capacity (26,29).
Type and duration of exercise
There was a wide variety of exercise programs used across the studies, most used a mixture of aerobic and resistance training with the exception of Dunne et al. (31), and the majority were able to show a significant increase in patient functional capacity following their interventions. The two studies that found no improvement in functional capacity were Yamamoto et al. (30) and Valkenet et al. (27). Yamamoto et al. (30) conducted a daily 2-week home-based program in sarcopenic elderly patients with the lowest reported compliance rate of 50%. It is likely that this particularly frail group of patients needed more hands-on involvement to enable them to complete the program as Mikami et al. (25) have shown that even with a 2-week program window, a meaningful improvement in patients can be attained. However, the Mikami et al. (25) program did require a 2-week hospital admission preoperatively, guaranteeing 100% compliance to daily exercise. Valkenet et al. (27) had a longer hospital-based program lasting up to 5 weeks, requiring two outpatient visits a week for a mix of aerobic and resistance training. On closer analysis, the average patient attendance was only 5.7 training sessions prior to having their operation. Given only half of these sessions were aerobic, it is not surprising they were unable to show any significant change in their cardiorespiratory functional assessments.
There is a growing body of evidence to show that the inclusion of aerobic exercise as part of a comprehensive PH program can result in significant improvements to patient functional capacity (26,29,46,47), but the type and duration of exercise is yet to be determined. From the six studies showing significant functional capacity improvement (25,26,28,29,31,32), the shortest time period required was 2 weeks as described above by Mikami et al. (25), but given that a 2-week hospital stint for all UGI cancer patients in not feasible, the next practical time period was 4–5 weeks conducted by Dunne et al. (31), Minnella et al. (32) and Nakajima et al. (28). The aerobic sessions required in each of these programs were all 3× weekly, using a mixture of high intensity interval training (HIIT), walking, cycling and jogging (28,31,32). These results appear to suggest that the type and intensity of aerobic exercise conducted is less important than the frequency of the sessions and the duration of the program. These studies in themselves are too small and heterogenous to definitively reach this conclusion and larger pragmatic multi-centred RCTs are needed, but this would open up the prospect of being able to design individualised PH programs utilising a variety of different exercise interventions to achieve maximum patient compliance.
The benefit of using resistance training, although it seems intuitive, is less clear (48). Five of the studies reporting an increase in functional capacity used some form of resistance training (25,26,28,29,32), however functional strength was only directly tested in one of these. Ngo-Huang et al. (26) conducted two functional strength tests; speed taken to do 5× sit-to-stands and hand grip strength using a handheld dynamometry. Their program was conducted over 16 weeks and found a significant improvement in the sit-to-stand time, but not handgrip strength. The theory behind including resistance training techniques in these PH programs is the increased anabolic stimulus you get from this particular mode of exercise. This should work to counteract the effects of NAC-induced sarcopenia by helping to build and maintain muscle and also by aiding the recovery of muscle function postoperatively (48,49). A recent systematic review looking at a wide variety of resistance training methods in the general population advised a program length of >6 weeks was required before any appreciable results are demonstrated (50). This program duration would likely only be achievable in most UGI cancer settings if it was started at the time of diagnosis as in Ngo-Huang et al. (26) and Halliday et al. (29). Unfortunately, due to the lack of direct testing in the other studies, it is difficult to form any conclusions as to the effectiveness of including resistance training in these PH programs.
Supervision and compliance
The studies in this review conducted a mix of both hospital (25,27,31) and home-based (26,28-30,32) exercise programs. Attendance to the hospital-based programs was significantly higher than the self-reported compliance during the home-based programs, with an overall attendance rate between 82–100% (25,27,31), compared to 50–86% in the home-based studies. A recent study comparing the two modes of delivery concluded that supervised programs result in a higher patient compliance and will therefore have better outcomes (51). However, significant improvements in functional capacity were also elicited in the home-based programs of this review with compliance rates of >80% in two studies (26,29). Three of the home-based studies used regular weekly or fortnightly telephone follow-ups to improve patient adherence to the program (26,29,32). Ngo-Huang et al. (26) also used accelerometers for up to 6 weeks during their 16-week program. The use of technology to assist in improving home-based compliance is ever evolving. From the recent exponential rise in video calling as a result of the COVID-19 pandemic, group sessions can now take place in the home more readily and apps/watches to track individual health data can provide real-time updates promoting increased activity and encouraging accountability (52,53). The home-based studies in this review have demonstrated that it is possible to improve functional capacity even with compliance rates as low as 63% (32), but more could be done to utilise the technology now widely available to try and increase compliance even further.
When analysing the compliance rates, it is important to note that almost all of the patients in these studies were self-selected. This is a study limitation as self-selected patients had a high level of motivation and wanted to participate in the exercise programs when they consented. Of all the patients eligible for inclusion in Valkenet et al. (27), 32% declined to take part. They analysed the baseline characteristics for the different groups and noted that those who refused lived further from the hospital (this was a hospital-based program) and had more severe systemic disease. Similarly high levels of patient refusal were seen in Dunne et al. of 57% and Minnella et al. of 40% (31,32), increasing the risk of confounding bias which could potentially skew the overall results. Dunne et al. (31) also noted that the patients starting their program with low functional capacity baselines had the most considerable gains in VO2 max and AT, hypothesising that it may be these more systemically unwell patients that stand to benefit the most from PH. This further supports the need for individualised PH programs, to promote inclusivity and encourage patient involvement.
Postoperative outcomes
All the studies included in this review were primarily designed to establish the feasibility of a PH program and/or the effects on patient functional capacity following them. None of the studies were adequately powered to assess postoperative outcomes, as such any conclusions inferred from these studies will need to be verified in further adequately powered RCTs.
Of the three studies that had a control group, the two RCTs (31,32) and the matched pair analysis (28), the two RCTs found no difference in postoperative outcomes whereas Nakajima et al. (28) observed a significant improvement in length of stay, but no difference in the incidence of major postoperative complications. This finding is interesting as it suggests that although some of the key risk factors for developing major complications (e.g., cancer stage and surgical complexity) may not be modifiable by simply increasing patient fitness, PH may result in a faster recovery from these complications when they do arise.
Given the particularly high rate of postoperative pulmonary complications in oesophageal cancer patients (54,55), Halliday et al. (29) monitored the incidence in their PH cohort. A significant correlation was observed between the amount of patient reported weekly physical activity and the risk of developing postoperative pneumonia. This has the potential to be a very significant finding in this cohort where the overall incidence of postoperative complications is up at 59% (56), and it will be interesting to see if these results can be replicated in further studies.
Only three studies looked at patient-centred outcomes using QoL measurement tools (26,31). Traditionally, it has been biomedical outcomes rather than QoL assessments that have been the principal endpoints in medical research (57). However, there is now an increasing drive to put patient-centred care at the forefront of new health innovations, particularly in cancer patients, with the aim of reducing the psychological toll of treatment. Dunne et al. (31) found a significant improvement in their PH group using the SF-36, a widely adopted tool designed to measure health related QoL. Dunne et al. (31) also noted that QoL in their control group did not change even when their fitness levels dropped, leading them to hypothesise that some of the QoL improvements may not be solely related to an improvement in fitness, but possibly through doing the training as a group with other participants in similar situations. However, contrary to Dunne et al. (31), Ngo-Huang et al. (26) did find a link between those least compliant with the program, who were more sedentary on the accelerometer, with lower QoL scores suggesting there is some correlation with fitness levels. QoL is an important outcome measure that should be used as standard in future studies. The highlighted variability of the current published work means it is important to understand the impacts of new PH programs on patient QoL as this will enable patient-centred improvements in the design and implementation process leading to higher compliance rates and ultimately more successful programs.
Multi-modal components
Four of the studies reviewed had nutritional components (26,28,30,32) to their PH programs and one had a psychological component (29). The nutritional components were all predominantly focused on high protein intake; two had leucine-rich amino acid supplements taken before and after exercise (28,30), one had a high protein meal post-exercise (26), and one had a high protein diet with additional whey protein supplements (32). Given the heterogenicity of the different methods used across the studies for monitoring their nutritional interventions, it is difficult to ascertain whether these supplements made any significant contribution to study outcomes. There is pre-existing evidence to suggest that protein supplementation could improve muscle strength and size during new exercise regimes (58,59), but these conclusions need to be more robustly investigated in the context of PH using validated nutritional assessment tools to accurately monitor the effects on this group of patients (60).
Halliday et al. (29) had an additional psychological component to their study. Patients were given sessions with a clinical nurse specialist where “the rationale for prehabilitation was reinforced, potential barriers and facilitators to exercise were explored and motivational interviewing techniques were used to facilitate positive behavioural change”. Unfortunately, there was no objective assessment carried out to determine how their patients reacted to this intervention or if it made any difference to overall patient compliance levels. This has again highlighted the need for valid outcome measurement tools to be incorporated into any study to enable accurate evaluations of each intervention implemented.
Limitations of this review
As a relatively new area of research, there is a paucity of large, pragmatic RCTs from which to extract data from and form conclusions. The studies reviewed in this paper were all small single centred studies with only two RCTs. The need for more robust RCTs is required to reduce the risk of selection bias, particularly in this self-selecting group of patients and to minimise the risk of confounding variables.
Although there are clear comparisons between the individual UGI sub-groups of low 5-year survival rates, high levels of sarcopenia and a growing use of neoadjuvant therapies which makes it useful for them to be reviewed together, there are also significant differences between these groups that would benefit from more detailed separate analysis. These include the degree of malnutrition on diagnosis, the types and treatment course of NAC, additional use of radiotherapy and therefore window of opportunity for which exercise PH would be most useful.
The data from these studies suggests that functional capacity can be improved through exercise PH programs, but none of these studies were adequately powered to evaluate if these changes in functional capacity are enough to affect outcomes. A large multi-centred trial is currently underway across the UK which has been designed to establish whether a PH exercise program ± psychological support can reduce postoperative length of stay in intra-cavity major cancer surgery (61). This study is aiming to recruit >1,500 patients to be adequately powered for their primary outcome. The results for this study are due in March 2022 and will hopefully go some way to answering some of the questions posed in this review.
This study was conducted as part of a Master’s dissertation and as such there was only one main reviewer in the study selection process. Although robust database searches were conducted at two different time intervals to reduce the risk of omitting eligible studies, two reviewers in the selection process would provide further assurance all studies were captured. The use of exclusion of non-English language studies is also a limitation.
Recommendations for future research
Larger multi-centred RCTs designed using a patient-centred pragmatic approach are required to fully evaluate some of the unanswered questions following this review, in particular:
- Does a significant change in preoperative functional capacity result in improved postoperative outcomes; including complications, length of stay and/or QoL?
- What is the optimal pragmatic duration and intensity of a PH exercise program?
- Can we utilise health data tracking technology to make home-based programs just as accessible as hospital-based programs to improve compliance?
- What is the optimal nutritional component of PH and how does it affect postoperative outcomes?
- What is the optimal psychological component of PH and how does it affect postoperative outcomes?
Conclusions
This systematic review has shown that it is feasible to conduct a PH program in UGI cancer patients which results in a significant improvement in functional capacity. It has also shown them to be feasible whilst patients are actively undergoing NAC treatment where it is found to be particularly effective at attenuating the usual functional decline. Whether a significant improvement in a patients’ preoperative functional capacity can enhance their postoperative outcomes is yet to be determined.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dmr.amegroups.com/article/view/10.21037/dmr-21-84/rc
Peer Review File: Available at https://dmr.amegroups.com/article/view/10.21037/dmr-21-84/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dmr.amegroups.com/article/view/10.21037/dmr-21-84/coif). CJ serves as an unpaid Associate Editor-in-Chief of Digestive Medicine Research from January 2022 to December 2023. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was submitted to the Brighton and Sussex Medical School Dissertation Committee for review on 8th June 2020 with full approval granted with no amendments required on the 2nd of July 2020. The review protocol can be made available on request.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wild CP, Weiderpass E, Stewart BW. World Cancer Report: Cancer Research for Cancer Prevention. International Agency for Research on Cancer (IARC) at the World Health Organisation (WHO), 2020.
- Types of Cancer. American Society of Clinical Oncology. Available online: https://www.cancer.net/cancer-types
- Maharaj AD, Holland JF, Scarborough RO, et al. The Upper Gastrointestinal Cancer Registry (UGICR): a clinical quality registry to monitor and improve care in upper gastrointestinal cancers. BMJ Open 2019;9:e031434. [Crossref] [PubMed]
- Sjoquist KM, Burmeister BH, Smithers BM, et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol 2011;12:681-92. [Crossref] [PubMed]
- Minnella EM, Drummond K, Carli F. The impact of prehabilitation on surgical outcomes. Ann Esophagus 2021;4:10. [Crossref]
- Jack S, West MA, Raw D, et al. The effect of neoadjuvant chemotherapy on physical fitness and survival in patients undergoing oesophagogastric cancer surgery. Eur J Surg Oncol 2014;40:1313-20. [Crossref] [PubMed]
- Kamarajah SK, Gujjuri RR, Elhadi M, et al. Elderly patients have increased perioperative morbidity and mortality from oesophagectomy for oesophageal cancer: A systematic review and meta-analysis. Eur J Surg Oncol 2021;47:1828-35. [Crossref] [PubMed]
- Szakmany T, Ditai J, Kirov M, et al. In-hospital clinical outcomes after upper gastrointestinal surgery: Data from an international observational study. Eur J Surg Oncol 2017;43:2324-32. [Crossref] [PubMed]
- Aloia TA, Zimmitti G, Conrad C, et al. Return to intended oncologic treatment (RIOT): a novel metric for evaluating the quality of oncosurgical therapy for malignancy. J Surg Oncol 2014;110:107-14. [Crossref] [PubMed]
- Ramos MFKP, de Castria TB, Pereira MA, et al. Return to Intended Oncologic Treatment (RIOT) in Resected Gastric Cancer Patients. J Gastrointest Surg 2020;24:19-27. [Crossref] [PubMed]
- Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med 2006;355:11-20. [Crossref] [PubMed]
- DePeralta DK, Ogami T, Powers B, et al. Completion, and not just initiation, of intended oncologic therapy is associated with improved survival after pancreatic resection for cancer. HPB 2018;20:S32. [Crossref]
- Finnerty DT, Buggy DJ. Return to intended oncologic therapy: a potentially valuable endpoint for perioperative research in cancer patients? Br J Anaesth 2020;124:508-10. [Crossref] [PubMed]
- Banugo P, Amoako D. Prehabilitation. BJA Education 2017;17:401-5. [Crossref]
- Richardson K, Levett DZH, Jack S, et al. Fit for surgery? Perspectives on preoperative exercise testing and training. Br J Anaesth 2017;119:i34-43. [Crossref] [PubMed]
- Scheede-Bergdahl C, Minnella EM, Carli F. Multi-modal prehabilitation: addressing the why, when, what, how, who and where next? Anaesthesia 2019;74:20-6. [Crossref] [PubMed]
- Waterland JL, McCourt O, Edbrooke L, et al. Efficacy of Prehabilitation Including Exercise on Postoperative Outcomes Following Abdominal Cancer Surgery: A Systematic Review and Meta-Analysis. Front Surg 2021;8:628848. [Crossref] [PubMed]
- Kitahata Y, Hirono S, Kawai M, et al. Intensive perioperative rehabilitation improves surgical outcomes after pancreaticoduodenectomy. Langenbecks Arch Surg 2018;403:711-8. [Crossref] [PubMed]
- Hughes MJ, Hackney RJ, Lamb PJ, et al. Prehabilitation Before Major Abdominal Surgery: A Systematic Review and Meta-analysis. World J Surg 2019;43:1661-8. [Crossref] [PubMed]
- Bolshinsky V, Li MH, Ismail H, et al. Multimodal Prehabilitation Programs as a Bundle of Care in Gastrointestinal Cancer Surgery: A Systematic Review. Dis Colon Rectum 2018;61:124-38. [Crossref] [PubMed]
- Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 2021;372: [Crossref] [PubMed]
- Health Education England (HEE) and National Institute for Healthcare and Excellence (NICE). NICE – Healthcare Databases Advanced Search. Available online: https://hdas.nice.org.uk
- Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [Crossref] [PubMed]
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in andomized trials. BMJ 2019;366:l4898. [Crossref] [PubMed]
- Mikami Y, Kouda K, Kawasaki S, et al. Preoperative In-Hospital Rehabilitation Improves Physical Function in Patients with Pancreatic Cancer Scheduled for Surgery. Tohoku J Exp Med 2020;251:279-85. [Crossref] [PubMed]
- Ngo-Huang A, Parker NH, Bruera E, et al. Home-Based Exercise Prehabilitation During Preoperative Treatment for Pancreatic Cancer Is Associated With Improvement in Physical Function and Quality of Life. Integr Cancer Ther 2019;18:1534735419894061. [Crossref] [PubMed]
- Valkenet K, Trappenburg JC, Schippers CC, et al. Feasibility of Exercise Training in Cancer Patients Scheduled for Elective Gastrointestinal Surgery. Dig Surg 2016;33:439-47. [Crossref] [PubMed]
- Nakajima H, Yokoyama Y, Inoue T, et al. Clinical Benefit of Preoperative Exercise and Nutritional Therapy for Patients Undergoing Hepato-Pancreato-Biliary Surgeries for Malignancy. Ann Surg Oncol 2019;26:264-72. [Crossref] [PubMed]
- Halliday LJ, Doganay E, Wynter-Blyth V, et al. Adherence to Pre-operative Exercise and the Response to Prehabilitation in Oesophageal Cancer Patients. J Gastrointest Surg 2021;25:890-9. [Crossref] [PubMed]
- Yamamoto K, Nagatsuma Y, Fukuda Y, et al. Effectiveness of a preoperative exercise and nutritional support program for elderly sarcopenic patients with gastric cancer. Gastric Cancer 2017;20:913-8. [Crossref] [PubMed]
- Dunne DF, Jack S, Jones RP, et al. Randomized clinical trial of prehabilitation before planned liver resection. Br J Surg 2016;103:504-12. [Crossref] [PubMed]
- Minnella EM, Awasthi R, Loiselle SE, et al. Effect of Exercise and Nutrition Prehabilitation on Functional Capacity in Esophagogastric Cancer Surgery: A Randomized Clinical Trial. JAMA Surg 2018;153:1081-9. [Crossref] [PubMed]
- Hollingsworth A, Danjoux G, Howell SJ. Cardiopulmonary exercise testing before abdominal aortic aneurysm surgery: a validated risk prediction tool? Br J Anaesth 2015;115:494-7. [Crossref] [PubMed]
- Older PO, Levett DZH. Cardiopulmonary Exercise Testing and Surgery. Ann Am Thorac Soc 2017;14:S74-83. [Crossref] [PubMed]
- Reed JL, Cotie LM, Cole CA, et al. Submaximal Exercise Testing in Cardiovascular Rehabilitation Settings (BEST Study). Front Physiol 2020;10:1517. [Crossref] [PubMed]
- Nordgren B, Fridén C, Jansson E, et al. Criterion validation of two submaximal aerobic fitness tests, the self-monitoring Fox-walk test and the Åstrand cycle test in people with rheumatoid arthritis. BMC Musculoskelet Disord 2014;15:305. [Crossref] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111-7. [Crossref] [PubMed]
- Antonescu I, Scott S, Tran TT, et al. Measuring postoperative recovery: what are clinically meaningful differences? Surgery 2014;156:319-27. [Crossref] [PubMed]
- Zugck C, Krüger C, Dürr S, et al. Is the 6-minute walk test a reliable substitute for peak oxygen uptake in patients with dilated cardiomyopathy? Eur Heart J 2000;21:540-9. [Crossref] [PubMed]
- Lee L, Schwartzman K, Carli F, et al. The association of the distance walked in 6 min with pre-operative peak oxygen consumption and complications 1 month after colorectal resection. Anaesthesia 2013;68:811-6. [Crossref] [PubMed]
- Keeratichananont W, Thanadetsuntorn C, Keeratichananont S. Value of preoperative 6-minute walk test for predicting postoperative pulmonary complications. Ther Adv Respir Dis 2016;10:18-25. [Crossref] [PubMed]
- Awdeh H, Kassak K, Sfeir P, et al. The SF-36 and 6-Minute Walk Test are Significant Predictors of Complications After Major Surgery. World J Surg 2015;39:1406-12. [Crossref] [PubMed]
- Hirabayashi R, Takahashi Y, Nagata K, et al. The validity and reliability of four-meter gait speed test for stable interstitial lung disease patients: the prospective study. J Thorac Dis 2020;12:1296-304. [Crossref] [PubMed]
- Navidi M, Phillips AW, Griffin SM, et al. Cardiopulmonary fitness before and after neoadjuvant chemotherapy in patients with oesophagogastric cancer. Br J Surg 2018;105:900-6. [Crossref] [PubMed]
- West MA, Loughney L, Lythgoe D, et al. Effect of prehabilitation on objectively measured physical fitness after neoadjuvant treatment in preoperative rectal cancer patients: a blinded interventional pilot study. Br J Anaesth 2015;114:244-51. [Crossref] [PubMed]
- Palma S, Hasenoehrl T, Jordakieva G, et al. High-intensity interval training in the prehabilitation of cancer patients-a systematic review and meta-analysis. Support Care Cancer 2021;29:1781-94. [Crossref] [PubMed]
- Carli F, Scheede-Bergdahl C. Prehabilitation to enhance perioperative care. Anesthesiol Clin 2015;33:17-33. [Crossref] [PubMed]
- Stephensen D, Hashem F, Corbett K, et al. Effects of preoperative and postoperative resistance exercise interventions on recovery of physical function in patients undergoing abdominal surgery for cancer: a systematic review of andomized controlled trials. BMJ Open Sport Exerc Med 2018;4:e000331. [Crossref] [PubMed]
- Cheema B, Gaul CA, Lane K, et al. Progressive resistance training in breast cancer: a systematic review of clinical trials. Breast Cancer Res Treat 2008;109:9-26. [Crossref] [PubMed]
- Krzysztofik M, Wilk M, Wojdała G, et al. Maximizing Muscle Hypertrophy: A Systematic Review of Advanced Resistance Training Techniques and Methods. Int J Environ Res Public Health 2019;16:4897. [Crossref] [PubMed]
- Awasthi R, Minnella EM, Ferreira V, et al. Supervised exercise training with multimodal pre-habilitation leads to earlier functional recovery following colorectal cancer resection. Acta Anaesthesiol Scand 2019;63:461-7. [Crossref] [PubMed]
- Argent R, Daly A, Caulfield B. Patient Involvement With Home-Based Exercise Programs: Can Connected Health Interventions Influence Adherence? JMIR Mhealth Uhealth 2018;6:e47. [Crossref] [PubMed]
- Laranjo L, Ding D, Heleno B, et al. Do smartphone applications and activity trackers increase physical activity in adults? Systematic review, meta-analysis and metaregression. Br J Sports Med 2021;55:422-32. [Crossref] [PubMed]
- Paul S, Altorki N. Outcomes in the management of esophageal cancer. J Surg Oncol 2014;110:599-610. [Crossref] [PubMed]
- Goense L, van Rossum PS, Tromp M, et al. Intraoperative and postoperative risk factors for anastomotic leakage and pneumonia after esophagectomy for cancer. Dis Esophagus 2017;30:1-10. [PubMed]
- Low DE, Kuppusamy MK, Alderson D, et al. Benchmarking Complications Associated with Esophagectomy. Ann Surg 2019;269:291-8. [Crossref] [PubMed]
- Haraldstad K, Wahl A, Andenæs R, et al. A systematic review of quality of life research in medicine and health sciences. Qual Life Res 2019;28:2641-50. [Crossref] [PubMed]
- Reule CA, Scholz C, Schoen C, et al. Reduced muscular fatigue after a 12-week leucine-rich amino acid supplementation combined with moderate training in elderly: a andomized, placebo-controlled, double-blind trial. BMJ Open Sport Exerc Med 2016;2:e000156. [Crossref] [PubMed]
- Morton RW, Murphy KT, McKellar SR, et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br J Sports Med 2018;52:376-84. [Crossref] [PubMed]
- Gillis C, Davies SJ, Carli F, et al. Current Landscape of Nutrition Within Prehabilitation Oncology Research: A Scoping Review. Front Nutr 2021;8:644723. [Crossref] [PubMed]
- The Wessex Fit-4-Cancer Surgery Trial (WesFit). NCT03509428. Available online: https://clinicaltrials.gov/ct2/show/NCT03509428
Cite this article as: Tyson EM, Malik M, Jones C. The effects of exercise prehabilitation in upper gastrointestinal oncology patients undergoing surgical resection: a systematic review. Dig Med Res 2022;5:11.


