
Jejunal diverticulitis: three case reports of a rare but clinically significant disease
Introduction
Acquired jejunal diverticulum is a rare, gastrointestinal condition having an estimated incidence from 0.42% to 2.3% when diagnosed through upper gastrointestinal imaging studies, and 0.3% to 4.6% at autopsy (1,2). By comparison, colonic diverticular disease is far more frequent, with an estimated prevalence between 50% to 66% in patients over the age of 80 (3). Diverticula frequently co-occur in other segments of the alimentary canal, with a rate of co-occurrence between colonic and jejunal diverticula somewhere between 35% to 75%, and between the jejunum and the urinary bladder in 12% of cases (4).
Jejunal diverticula typically occur in patients aged 60 years old and above (5). The exact mechanism of its pathogenesis is still not known, but it seems to be related to dysfunctional smooth muscle layers or the myenteric plexus, with subsequent abnormalities in peristalsis leading to increased intraluminal pressure and diverticulum formation (6). The initial case series was published by Osler in 1881 and while diagnostics have improved with advanced endoscopic technique, this disease remains to be a challenging diagnosis in some cases (1,5). Complications not directly associated with diverticulitis may also occur, namely hemorrhage, obstruction, and biliary disorders, as identified in a recent literature review (7).
The rarity of the disease may render it low on a clinician’s differential, meanwhile, the potential for severe complications to arise from seemingly benign clinical presentations make it a worthwhile topic for discussion.
We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/dmr-20-161).
Case presentation 1
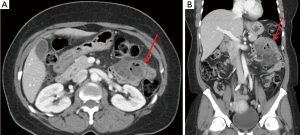
A 55-year-old female presented to the emergency department with abdominal pain and fever. She was in her usual state of health until two days prior to presentation, when she developed severe back and thoracic pain, which began to radiate to the left upper quadrant of the abdomen with tenderness to palpation, and was not relieved with over-the-counter analgesics. She reported mild nausea over the past two days with associated anorexia, without vomiting or changes in bowel habits. Her fever developed overnight and persisted up to the time of presentation. History is notable for carcinoma of the breast, currently being treated. Past surgical history is notable for a caesarean section. Physical examination of the abdomen reveals normal bowel sounds, no clear peritoneal signs, and significant left upper quadrant tenderness to palpation. Initial laboratory studies revealed a leukocytosis and mild anemia. A CT scan of the abdomen and pelvis performed with intravenous contrast showed a 2 cm diverticulum arising from the mesenteric border of the proximal jejunum with surrounding inflammation and the suspicion of micro perforation (Figure 1). Despite the localized perforation on CT scan, rather than conservative management, the decision was made to take the patient to the operating room for exploratory laparotomy given that the patient had persistent, severe pain not relieved by pain medication with associated tachycardia. At approximately 15 cm distal to the ligament of Treitz, there was an indurated portion of jejunum containing a sealed-off perforated diverticulum. There was no gross evidence of ischemia of the small bowel upon gross inspection, and there was no other diverticulum in the jejunum. The decision was made to resect approximately 16 cm of small bowel with primary anastomosis, and the specimen was sent for pathology. Pathology showed jejunal diverticulum with abscess and perforation. The patient tolerated the procedure well and there were no postoperative complications. She was discharged home postoperatively on day four.
Case presentation 2
A 76-year-old female presented with a 3-month history of abdominal pain, shortness of breath, and productive cough. Examination of her abdomen revealed moderate focal tenderness to palpation in the epigastric and left upper quadrant region, distension, and tympany to percussion. Her history is significant for jejunal diverticulitis with conservative management 4 years prior and jejunal diverticulectomy due to diverticular perforation. At that time, she had radiographic pneumoperitoneum and pneumatosis intestinalis on CT scan imaging. On this admission, she had a chest X-ray and abdominal CT showing massive pneumoperitoneum. On abdominal CT, there was evidence of multiple perforated jejunal diverticula. The patient underwent emergent exploratory laparotomy. During the operation, approximately 20 large scattered jejunal diverticula were found on the mesenteric border starting at approximately 1 foot distal to the ligament of Treitz extending for 110 cm (Figure 2). She had 3–4 jejunal diverticula that were 5–7 cm in diameter with massive crepitance and associated air in the mesentery. Two of those jejunal diverticula had micro perforations without spillage of enteric contents. An en bloc small bowel resection of 110 cm was performed since the large jejunal diverticula were scattered along that segment and the patient was found to have redundant small intestine and colon. Laparotomy also revealed that the patient had co-existing small (~2 cm diameter), non-inflamed colonic diverticula, which were left undisturbed. Pathology revealed jejunal diverticulosis with ruptured diverticulum. The patient had an unremarkable postoperative course, and was discharged home on postoperative day number five. She was seen postoperatively in the clinic for staple removal, and was still doing well on her 4-week postoperative visit.

Case presentation 3
A 76-year-old male presented with a 4-day history of abdominal pain and worsening lethargy. The patient has several medical comorbidities and had a small bowel resection 4 months prior for jejunal diverticulitis. He presented tachycardic, febrile, and quickly became profoundly hypotensive. He had a CT scan of the abdomen and pelvis that showed pneumatosis intestinalis within small bowel loops just proximal to the previous anastomosis with a mesenteric fluid collection. He had severe sepsis and was resuscitated in the intensive care unit for a short period of time prior to the operating room. He underwent an urgent exploratory laparotomy. He was found to have extensive jejunal diverticulosis extending nearly to the ligament of Treitz (Figure 3). He had a perforated jejunal diverticulum into the mesentery with mesenteric abscess formation. Near the prior small bowel anastomosis, there was also noted to be inflamed mesentery with a large pus-containing abscess. A large segment of the jejunum was resected including all the diverticula grossly identified and a primary anastomosis performed, measuring approximately 75 cm long. Pathology revealed acute jejunal diverticulitis with serositis and microabscesses as well as an anastomotic site with disarrayed muscularis propria. Postoperatively, he had a prolonged course in the intensive care unit for resuscitation and required long term intravenous antibiotics for anaerobic intraabdominal infection, and parenteral nutrition. He suffered a complication of fascial dehiscence and did require re-operation. Since the patient had several comorbidities, was on chronic steroids, and had a possible malnutrition that could be connected to his previous long segment resection, these factors combined may have contributed to the dehiscence. One potential solution for preventing dehiscence is to perhaps start him on total parenteral nutrition in the early postoperative period. He progressed to tolerating a low residue oral diet and was ultimately discharged to a skilled nursing facility on hospital day 27.

Discussion
For a disease process that is relatively rare, these three patients presented all within one month of each other at our institution. There is a significant diagnostic challenge associated with jejunal diverticula due to its varied presentation as with all our cases (7). It can mimic other disease symptomatology as in appendicitis, colonic diverticulitis, and Crohn’s disease (8). Collectively, all cases included left upper quadrant and epigastric pain, shortness of breath, fever, and lethargy. Nonspecific symptoms such as upper abdominal pain, nausea, bloating or anorexia were also noted in these patients (9). The clinical timeline ranged from a four-day acute event with severe abdominal pain to a slowly progressing, four-year asymptomatic presentation which are patients’ number one and two, respectively. Concurrent colonic diverticula are also a common finding in patients and all three had this condition.
Definitive diagnosis of jejunal diverticulosis is usually not made until exploratory surgery. Despite an improvement in imaging techniques, some of these lesions could be challenging to identify as the ostia of large diverticula can easily empty while smaller lesions could be too small to retain or be filled if at all (9-11). Other clinical findings that may hinder accuracy in diagnosis is the presence of extradigestive gas without perforation and lesions with pseudo-ischemic presentations such as enteroliths or bowel obstruction (12). Despite this, CT remains to be the imaging of choice for suspected jejunal diverticulosis. Findings that are most consistent with confirmed jejunal diverticulosis are inflammatory diverticula, thick enhancing intestinal wall, and extraluminal gas or fluid (12). In a retrospective chart review, radiologists were able to correctly identify jejunal diverticulosis in 75% of all the patients studied (13). The role of magnetic resonance for diagnosis is also helpful as an imaging modality on a non-emergent basis and if the CT imaging findings are inconclusive, however there is lack of evidence for evaluating the use of MRI for jejunal diverticulosis (14,15).
Optimal management of jejunal diverticulitis is also not well defined, although treatment algorithms have been proposed (15-17). Lebert et al. reported a modified Hinchey classification of jejunoileal diverticulitis that was adapted from Kaiser et al. There are four disease stages, namely, stage Ia is confined peri jejunoileal inflammation or phlegmon, Ib is confined peri jejunoileal abscess, stage II is distant mesenteric abscess, and stage III is generalized purulent peritonitis (12). Gross diverticular perforation was noted in all three patients. Intraluminal abscess formation was found in patient number one and local mesenteric abscess with serositis was found in patient number three, both of which are classified as stage Ia. Despite having extensive perforated diverticula, in this classification patient number two is categorized as stage Ib. In a retrospective review of 9 patients with complicated jejunal diverticulitis, Schloericke et al. determined that multiple diverticula (more than 3) or free perforation with peritonitis was an indication for segmental resection, with 7 out of 9 patients in their study requiring segmental resection for intraoperative findings including peritonitis, multiple diverticula, and perforation (9). These indications were used as our guiding principles for our operative decision making. Despite patient number one being classified as stage Ia, the patient presented with severe pain unresponsive to analgesia and associated tachycardia prior to the operation. Patient number two had stage Ib disease and presented with complicated, recurrent jejunal diverticulitis. At the time of index operation, single diverticulectomy was performed leaving the unperforated extensive diverticulosis within. Four years after, the patient presented to us with chronic pneumoperitoneum without peritonitis, similar to the description by Harbi et al. (15). Patient number three also has stage Ia disease but the patient also had significant hypotension and signs of early sepsis after meeting SIRS criteria four months status post small bowel resection. Similar to patient number two, resection was limited only to the segment that had active jejunal diverticulitis. As for patients’ two and three, perhaps the existing segment with several inactive diverticula that was not resected may increase the risk of diverticulitis recurrence with complications. It can be postulated that if both patients had complete large segmental resection at the time of index operation, perhaps the second operation could have been avoided as supported by the proposed algorithm by Harbi et al. (15). Because of the rarity of this condition however, the exact mechanism and rate of recurrence is not known. There are no best practice guidelines because of how rare this disease is. A report from Leigh et al. showed that there were only 53 case reports on jejunal diverticulosis within the past decade (18). Of the other three published case series in the English literature, our paper describes a case series on jejunal diverticulosis from a single institution in North America that reported favorable outcomes with definitive operative management (19-21).
Conclusions
Jejunal diverticulum is a rare disease that warrants heightened awareness since complications such as perforations can result in high morbidity and mortality if not recognized promptly. Since definitive diagnosis is made intraoperatively, CT scan and a careful history and physical must be obtained. CT scan of the abdomen and pelvis is the diagnostic tool of choice as it can identify a jejunal diverticulum in a majority of cases and help determine disease extent and the presence of complications. When feasible, complete segmental resection of jejunal diverticula should be performed especially in patients with multiple diverticula (more than 3), perforation, or peritonitis in order to prevent disease recurrence.
Acknowledgments
Funding: None.
Footnote
Reporting Checking: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/dmr-20-161
Peer Review File: Available at http://dx.doi.org/10.21037/dmr-20-161
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr-20-161). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from all three patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wilcox RD, Shatney CH. Surgical implications of jejunal diverticula. South Med J 1988;81:1386-91. [Crossref] [PubMed]
- Cooke WT, Cox EV, Fone DJ, et al. The clinical and metabolic significance of jejunal diverticula. Gut 1963;4:115-31. [Crossref] [PubMed]
- Matrana MR, Margolin DA. Epidemiology and pathophysiology of diverticular disease. Clin Colon Rectal Surg 2009;22:141-6. [Crossref] [PubMed]
- Kassir R, Boueil-Bourlier A, Baccot S, et al. Jejuno-ileal diverticulitis: etiopathogenicity, diagnosis and management. Int J Surg Case Rep 2015;10:151-3. [Crossref] [PubMed]
- Palder SB, Frey CB. Jejunal diverticulosis. Arch Surg 1988;123:889-94. [Crossref] [PubMed]
- Krishnamurthy S, Kelly MM, Rohrmann CA, et al. Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus. Gastroenterology 1983;85:538-47. [Crossref] [PubMed]
- Rangan V, Lamont JT. Small Bowel Diverticulosis: Pathogenesis, Clinical Management, and New Concepts. Curr Gastroenterol Rep 2020;22:4. [Crossref] [PubMed]
- Alam S, Rana A, Pervez R. Jejunal diverticulitis: imaging to management. Ann Saudi Med 2014;34:87-90. [Crossref] [PubMed]
- Schloericke E, Zimmermann MS, Hoffmann M, et al. Complicated jejunal diverticulitis: a challenging diagnosis and difficult therapy. Saudi J Gastroenterol 2012;18:122-8. [Crossref] [PubMed]
- Fidan N, Mermi EU, Acay MB, et al. Jejunal Diverticulosis Presented with Acute Abdomen and Diverticulitis Complication: A Case Report. Pol J Radiol 2015;80:532-5. [Crossref] [PubMed]
- Kwak JY, Park EH, Park CS, et al. Uncomplicated jejunal diverticulosis with pneumoperitoneum. Ann Surg Treat Res 2016;90:346-9. [Crossref] [PubMed]
- Lebert P, Millet I, Ernst O, et al. Acute Jejunoileal Diverticulitis: Multicenter Descriptive Study of 33 Patients. AJR Am J Roentgenol 2018;210:1245-51. [Crossref] [PubMed]
- Fintelmann F, Levine MS, Rubesin SE. Jejunal diverticulosis: findings on CT in 28 patients. AJR Am J Roentgenol 2008;190:1286-90. [Crossref] [PubMed]
- Transue DL, Hanna TN, Shekhani H, et al. Small bowel diverticulitis: an imaging review of an uncommon entity. Emerg Radiol 2017;24:195-205. [Crossref] [PubMed]
- Harbi H, Kardoun N, Fendri S, et al. Jejunal diverticulitis. Review and treatment algorithm. Presse Med 2017;46:1139-43. [Crossref] [PubMed]
- Baskin RH Jr, Mayo CW. Jejunal diverticulosis; a clinical study of 87 cases. Surg Clin North Am 1952;1185-96. [Crossref] [PubMed]
- Ramistella AM, Brenna M, Fasolini F, et al. Jejuno-ileal diverticulitis: A disorder not to underestimate. Int J Surg Case Rep 2019;58:81-4. [Crossref] [PubMed]
- Leigh N, Sullivan BJ, Anteby R, et al. Perforated jejunal diverticulitis: a rare but important differential in the acute abdomen. Surg Case Rep 2020;6:162. [Crossref] [PubMed]
- Ghandour R, Khalifeh G, Orm NB, et al. Jejunal diverticular disease: a report of three cases. J Surg Case Rep 2020;2020:rjaa472.
- Patel B, Basil A, Cave DR. A Case Series of Jejunal Diverticulosis: A Variety of Presentations: 2191. Off J Am Coll Gastroenterol ACG 2016;111:S1047.
- Karas L, Asif M, Chun V, et al. Complicated small bowel diverticular disease: a case series. BMJ Case Rep 2017;2017:bcr2017219699 [Crossref] [PubMed]
Cite this article as: Sogunro OA, Buck M, Labrias PR. Jejunal diverticulitis: three case reports of a rare but clinically significant disease. Dig Med Res 2021;4:39.


