
Robotic resection of retroperitoneal paraganglioma mimicking a hepatic mass: a case report
Introduction
Paragangliomas are extra-adrenal, non-epithelial neuroendocrine tumors of the paraganglia arising from multiple sites throughout the head, neck, thorax, and abdomen. They make up 22% of pheochromocytomas (1). Primary hepatic paragangliomas are extremely rare, and hepatic metastasis from an adrenal primary are more common (2). These tumors can mimic primary hepatocellular carcinomas or secondary neuroendocrine metastases on imaging. This report aims to describe the robotic resection of a large paracaval retroperitoneal paraganglioma mimicking a primary hepatic lesion on preoperative imaging. We present the following case report describing a unique presentation of a retroperitoneal paraganglioma and description of its robotic resection in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/dmr-20-71).
Case presentation
Preoperative evaluation
A 62-year-old man with long standing history of hypertension who was referred to our facility for management of biopsy proven intrahepatic neuroendocrine tumor. He was noted, on routine physical lab exam performed by his Primary care physician, to have elevated serum bilirubin at 1.7 mg/dL and alkaline phosphatase at 94 U/L. He underwent a dedicated RUQ US which revealed a 6.9 cm mass in segment 2 of the liver. Percutaneous liver biopsy of the mass appeared to be consistent with a neuroendocrine tumor with immunohistochemistry (IHC) positive for CD117 (C-kit), synaptophysin, chromogranin, and CD56, and negative for pancytokeratin (AE1/AE3). Laboratory studies revealed elevated serum chromogranin A [832 ng/mL, normal (n) <93], normetanephrines (18.9 nmol/L, n<0.89) and normal alpha fetoprotein (<5.0 ng/mL, n<8.5). Given these findings, he was referred to our facility for further workup and management. In addition to the above, our history and physical revealed he had no abdominal pain, diarrhea, nausea, vomiting, tachycardia, headache, perspiration, palpitations, pallor, weight loss, or loose stools. However, he had hypertension controlled on Atenolol and Hydrochlorothiazide for over 10 years. Of note, he reportedly had hypertension during his biopsy at the outside hospital requiring a dose of hydralazine. His surgical history is also notable for laparoscopic cholecystectomy about 10 years prior where a liver mass was seen intraoperatively, however, he was lost to follow up post-operatively.
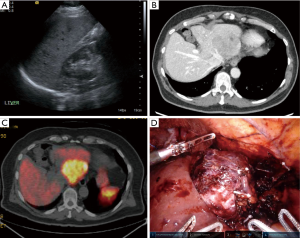
Cross sectional imaging to better characterize the mass included CT chest, abdomen, and pelvis and 68Ga dotatate PET. His abdominal imaging revealed a heterogenous enhancing lesion measuring 7.3 cm ×7.0 cm, centered in the left lateral segment involving segments 2, 3 and 4b with maximum standardized uptake value (SUV) of 16.1 with no disease dissemination noted. The mass appeared to be invading the left lateral segment of the liver, abutting the left anterolateral aspect of the inferior vena cava (IVC) and compress the left hepatic vein (Figure 1A,B,C). Other studies included an upper and lower endoscopy which did not show any lesions. Thus, diagnosis favored a primary hepatic neuroendocrine tumor, and was offered a robotic approach to resection. Given his known history of hypertension and nature of his tumor, he was also referred to endocrinology for preoperative optimization. Phenoxybenzamine was added to his regimen and he was weaned off his hydrochlorothiazide to provide both alpha and beta blockade for 14 days before resection. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Intraoperative approach
Access to the peritoneal cavity was achieved via a supraumbilical incision using the Hassan technique with a 12 mm AirSeal port. After insufflation, omental adhesions were taken down from the abdominal wall laparoscopically to sequentially place four 8 mm robotic ports in the left and right subcostal position. In reverse Trendelenburg and partial left lateral decubitus position, the Xi daVinci robot (intuitive surgical, was docked from the patient’s left side. It was confirmed that the anesthesia team was prepared to manage intraoperative hypertensive crisis. His intraoperative hypertension was managed with labetolol.
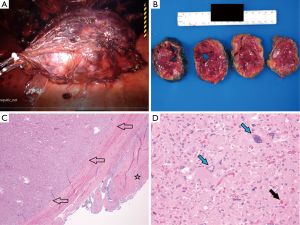
Intraoperative ultrasound was performed to demonstrate the tumor and its relationship to the surrounding vasculature. We began the resection by taking down the left triangular ligament. There were dense inflammatory adhesions between the tumor and left diaphragmatic crus. During the dissection, it became apparent the tumor was arising from the retroperitoneum and not the liver. There were parasitized vascular pedicles off the phrenic vessels controlled with hem-o-lok clips and monopolar shears. The left lateral sector of the liver was retracted anterolaterally. There were more blood vessels parasitized from the liver parenchyma supplying the tumor which were small and friable, controlled with small titanium clips. The friability made resection challenging, oftentimes requiring direct repair with 3-0 polysorb and 4-0 prolene sutures on the hepatic side of resection bed. After detachment from the diaphragm and retroperitoneum, it was apparent that inflow to the tumor was off the left portal structures and outflow into the left hepatic vein and IVC directly. Inflow was controlled with hemolock clips. Outflow into the IVC was controlled using 3-0 polysorb sutures and EndoGIA stapler with a 45 mm vascular load. The tumor was attached to segment 2 which required a wedge resection to remove using a crush clamp technique with cadiere graspers and monopolar shears (Figure 1D). There was an unavoidable venotomy over the IVC which was repaired with 4-0 prolene sutures. The surgical bed was examined, confirming complete hemostasis and lack of bile or chyle leak. The tumor was placed in an EndoCatch bag, and the specimen was removed through an extension of the assistant port incision, and sent to pathology (Figure 2A). The estimated blood loss was 500 milliliters and operative time was 220 minutes from docking of the robot to removal of the specimen.
Post-operative management and follow-up
Given his wedge hepatic resection, he had 2 sequential laboratory evaluation of his coagulation and hematocrit as part of our robotic hepatectomy pathway. The patient had transient mild hypotension with systolic blood pressures in the 90s but otherwise did well post-operatively, and was discharged on post-operative day 1. He was seen in clinic on post-operative day 12, doing well with excellent pain control, well healing incisions and without complaints. He continues to be off his antihypertensives. Gross examination of the specimen revealed an 8.6 cm tumor (Figure 2B, with a somewhat soft, friable center. Histologic examination shows that the tumor is comprised of sheets and nests of large cells with abundant eosinophilic cytoplasm, nuclear pleomorphism and occasional prominent nucleoli. Occasional large “bizzare” nuclei can be seen at scanning magnification. Extracellular eosinophilic globules or spherules are seen throughout the tumor (Figure 2C,D). No necrosis is identified, and the mitotic rate is low. The histomorphologic features are in keeping with a paraganglioma.
Discussion
Extra-adrenal paragangliomas behave more aggressively than their adrenal counterparts with metastasis occurring in 20–70% of cases (3). They are classically associated with the organ of Zuckerandl though other common locations include the infradiaphragmatic para-aortic region and mediastinum (3). Unusual sites of origin include peri-adrenal, interaortocaval, and paracaval retroperitoneal sites, as well as tumors in organs where they may not be expected in the differential diagnosis of neuroendocrine neoplasms, such as thyroid, parathyroid, pituitary, gut, pancreas, liver, mesentery, lung and heart (4). Paragangliomas at unusual anatomic locations can present a diagnostic challenge with multifocal lesions sometimes reported as paraaortic lymphadenopathy (4). The above case demonstrates a paracaval paraganglioma invading the left lateral segment of the liver. Most of the mass was encased by the left lateral segment without a clear connection to the retroperitoneum on imaging thus the diagnosis of primary hepatic paraganglioma was initially made.
Additionally, dispersed microscopic paraganglia associated with components of the autonomous nervous system in the liver and lung make them rare but possible sites of primary paraganglioma. Metastatic lesions should be considered at sites where normal chromaffin tissue is not present (4). The bilateral adrenal glands were intact on computed tomography thus the possibility of metastatic pheochromocytoma was ruled out. Biopsy results was consistent with neuroendocrine differentiation. There was the benefit of pathologic diagnosis preoperatively however biochemical diagnosis in addition to imaging is key to making a diagnosis (3). It should be noted that the necessity and safety of biopsy before surgery requires further investigation as surgical resection is usually the next step after biochemical diagnosis and imaging. Biopsy could lead to rupture, bleeding or hypertensive crisis (5).
Patients may present with catecholamine excess including paroxysmal hypertension, headache, palpitation and sweating or may be completely asymptomatic (6). In this case, the patient had a history of hypertension, controlled well on atenolol and hydrochlorothiazide for over ten years before presentation. Preoperative alpha blockade is critical and recommended, I our case, phenoxybenzamine was used. He did have an isolated hypertensive event at the time of biopsy done at the outside hospital which is likely due to catecholamine release. Furthermore, the resolution of his hypertension post operatively without antihypertensives points to the cause of his hypertension.
Robotic resection of large (>5 cm) retroperitoneal paragangliomas is limited in literature (7). Xia et al. (7), was the first series to describe 4 cases of robotic resection of retroperitoneal paraganglioma. Laparoscopic approach can be challenging for resection of retroperitoneal paragangliomas given the posterior location limiting exposure, the anatomic variations, rich vascularization, and the potential for hemodynamic instability due to manipulation. Liu et al. in a series with 25 patients involving benign, non-adrenal retroperitoneal tumors describes the safety and feasibility of robotic resection of retroperitoneal tumors without adverse outcomes. In addition to improved visibility, advantages over laparoscopy were credited to precision of dissection and improved dexterity. In our case, this allowed for better visualization and prompt control of small and large size blood vessels feeding and draining the mass and liver parenchyma to achieve complete hemostasis. The additional range of motion afforded by the robotic platform allowed for routine suture control of bleeding on the hepatic bed and even repair of a small venotomy on the IVC (8). Overall, it allowed the minimally invasive resection of this large retroperitoneal mass, aiding in expedited recovery and minimal hospital length of stay. This is the first study to describe robotic resection of a large retroperitoneal mass invading the liver requiring a concomitant partial hepatectomy.
Conclusions
Paragangliomas involving the left lateral segment of the liver should be further investigated for a retroperitoneal primary. The robotic platform is a versatile and effective minimally invasive approach that allows for resection of both primary hepatic and paracaval paragangliomas.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/dmr-20-71
Peer Review File: Available at http://dx.doi.org/10.21037/dmr-20-71
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr-20-71). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Khan MR, Raza R, Jabbar A, et al. Primary non-functioning paraganglioma of liver: a rare tumour at an unusual location. J Pak Med Assoc 2011;61:814-6. [PubMed]
- Lin CS, Hsu YH. A primary paraganglioma of the liver mimicking hepatocellular carcinoma. Ci Ji Yi Xue Za Zhi 2019;31:286-8. [PubMed]
- Baez JC, Jagannathan JP, Krajewski K, et al. Pheochromocytoma and paraganglioma: imaging characteristics. Cancer Imaging 2012;12:153-62. [PubMed]
- Asa SL, Ezzat S, Mete O. The Diagnosis and Clinical Significance of Paragangliomas in Unusual Locations. J Clin Med 2018;7:280. [Crossref] [PubMed]
- Liao W, Ding ZY, Zhang B, et al. Primary functioning hepatic paraganglioma mimicking hepatocellular carcinoma: A case report and literature review. Medicine (Baltimore) 2018;97:e0293. [Crossref] [PubMed]
- You Z, Deng Y, Shrestha A, et al. Primary malignant hepatic paraganglioma mimicking liver tumor: A case report. Oncol Lett 2015;10:1176-8. [Crossref] [PubMed]
- Xia L, Xu T, Wang X, et al. Robot-assisted laparoscopic resection of large retroperitoneal paraganglioma - initial experience from China. Int J Med Robot 2016;12:686-93. [Crossref] [PubMed]
- Liu Q, Gao Y, Zhao Z, et al. Robotic resection of benign nonadrenal retroperitoneal tumors: A consecutive case series. Int J Surg. 2018;55:188-92. [Crossref] [PubMed]
Cite this article as: Afolayan O, Mau B, Park J. Robotic resection of retroperitoneal paraganglioma mimicking a hepatic mass: a case report. Dig Med Res 2020;3:71.


