
Gallbladder herniation and cholecystitis within a parastomal hernia: a case report and literature review
Introduction
Parastomal herniation is a common occurrence following stoma creation. Depending on the type of stoma created, the incidence of parastomal hernias ranges widely between 0 and 48.1%; occurring more frequently in individuals with end colostomies (1). Reports of gallbladder herniation, however, are few and far between with both surgical and non-surgical options documented.
In this paper, we outline a case of gallbladder herniation within a parastomal hernia with associated cholecystitis and pancreatitis. Existing literature was reviewed and their therapeutic approaches examined to explore the optimal treatment for this uncommon presentation. We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/dmr-20-82).
Case presentation
A 63-year-old lady presented with abdominal pain and vomiting secondary to gallbladder parastomal herniation complicated by cholecystitis and pancreatitis. Her medical history includes congenital mental subnormality and perforated diverticulitis in 2014, necessitating an open subtotal colectomy and end ileostomy creation. She developed a parastomal hernia a year after her surgery, which was conservatively managed as the patient was asymptomatic.
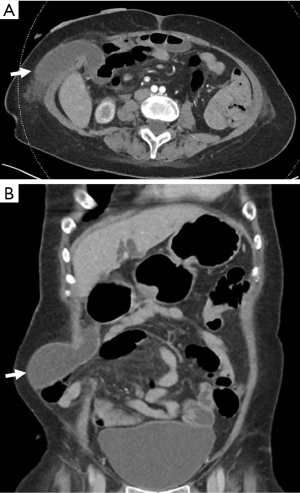
She presented in January 2020 with epigastric discomfort and vomiting with abdominal examination revealing a tender epigastrium and an otherwise healthy stoma with associated parastomal hernia. Investigations revealed raised serum amylase of 156 U/L and neutrophilia on full blood count. Computed tomography (CT) of the abdomen showed a herniated gallbladder in the parastomal hernia with groove pancreatitis. The patient was managed conservatively with fluids and bowel rest as her family declined any surgical intervention. She was discharged well after a week of hospitalisation but returned soon after with recurrent abdominal pain and fever. Serum amylase and alkaline phosphatase were elevated with neutrophilia on full blood count. A repeat CT showed recurrent pancreatitis, a dilated common bile duct (CBD) with new pericholecystic stranding suggestive of acute cholecystitis (Figure 1).
The patient’s family was counselled and agreeable with surgery given a repeated presentation and deteriorating clinical condition from the initial admission. The patient was started on broad spectrum antibiotics and underwent a midline laparotomy, intraoperative cholangiogram (IOC), cholecystectomy and parastomal hernia repair using a biological Permacol (Covidien, Mansfield, USA) mesh. Intra-operatively, the gallbladder had herniated within the parastomal hernia with a fascial defect of 4cm. IOC revealed a dilated CBD with no filling defects. The fascial defect was repaired primarily followed by the Sugarbaker technique of intraperitoneal onlay Permacol mesh application (Figure 2). Her recovery was complicated by hospital acquired pneumonia for which she completed a course of antibiotics. She remains well to date, 5 months after surgery, with no hernia recurrence.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s legal guardian. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Discussion
The management of parastomal hernias remains debatable. Significant morbidity with high recurrence rates between 37–76% questions the utility of an aggressive surgical approach (2,3). A variety of surgical techniques, including primary fascial repair, mesh repair and stoma relocation, have been performed with varying outcomes; though little is known of their application in cases of parastomal hernias complicated by gallbladder herniation.
Existing literature was reviewed with 10 reported cases of gallbladder parastomal herniation (Table 1) (4-13). Including our case, the median age of presentation was 73.5 years old (range, 50–88) with a preponderance of female patients (81.8%). Eight patients underwent open surgical intervention (7 cholecystectomies, 6 hernia repairs), 2 patients underwent manual hernia reduction and 1 patient was managed conservatively. Of the hernia repairs, 2 were repaired primarily while 4 others received a mesh repair (2 biological mesh, 1 synthetic, 1 not reported). All patients were discharged well with no stoma recurrence with the exception of Rashid et al. reporting subsequent recurrence at 20 months and stoma resited.
Table 1
| Year of publication | Age/gender | Type of stoma | Clinical presentation | Significant laboratory results | Treatment | Outcome |
|---|---|---|---|---|---|---|
| 2005; (4) | 73/female | Ileal conduit | Incarcerated gallbladder | ↑ WBC; ↑bilirubin | Laparotomy, cholecystectomy and primary hernia repair | No recurrence |
| 2005; (5) | 63/female | Transverse colostomy | Abdominal pain and nausea | Normal bilirubin | Manual reduction | No recurrence after 16 months |
| 2009; (6) | 74/female | End ileostomy | Small bowel obstruction secondary to incarcerated hernia | ↑ WBC ↑bilirubin | Laparotomy, cholecystectomy and hernia mesh repair (mesh material not mentioned) | Recurred after 20 months with stoma resited |
| 2013; (7) | 76/male | End ileostomy | Abdominal pain | ↑ WBC; ↑creatinine | Laparoscopic converted to open surgical detorsion and cholecystectomy; hernia repair not reported | Discharged well, follow up not reported |
| 2015; (8) | 85/female | Ileal conduit | Abdominal pain and fever | ↑ WBC | Laparotomy, cholecystectomy; hernia not repaired | Patient well at 1 month |
| 2017; (9) | 50/female | Right hypochondrium diverting colostomy | Abdominal pain and vomiting | Not reported | Right subcostal laparotomy, cholecystectomy and primary hernia repair | Discharged well, follow up not reported |
| 2017; (10) | 88/female | Transverse loop colostomy | Abdominal pain and fever | ↑ WBC | Manual reduction | Discharged well, follow up not reported |
| 2017; (11) | 89/male | Diverting loop ileostomy | Abdominal pain and nausea | ↑ Neutrophils | Conservative management | Discharged well, follow up not reported |
| 2018; (12) | 63/female | End transverse colostomy | Abdominal bloating | ↑ Neutrophils | Colostomy takedown, ascending colon to rectal anastomosis, cholecystectomy, appendectomy and abdominal wall reconstruction with bioprosthetic onlay mesh | No recurrence at follow up, duration not stated |
| 2019; (13) | 75/female | End ileostomy | Abdominal pain and nausea | Not reported | Lateral transverse incision, reduction of gallbladder and onlay hernia repair with synthetic mesh | No recurrence after 6 months |
WBC, white blood cell.
In spite of high recurrence rates, parastomal hernias warrant surgical intervention for those who develop complications from the hernia or whose quality of life is affected by the hernia. In the case of gallbladder parastomal herniation, gallbladder inflammation or incarceration necessitates surgical intervention and complicates repair in a potentially contaminated surgical field.
Primary fascial repair, stoma relocation and mesh repair are some of the techniques for parastomal hernia repairs. Whilst a simple technique with limited morbidity, direct fascial repair has limited longevity with exceedingly high recurrence rates of 59–69.4%, unacceptable by today’s standards (14-16). The comparatively shorter and less morbid procedure may, however, apply to individuals with a poor premorbid state and limited lifespan or in those whom prosthetic reinforcement may be contraindicated. On the other hand, stoma relocation has lower recurrences of 26.4–29% but poses greater morbidity with a prolonged operation and puts the new stoma and previous stoma site at risk of another herniation, potentially resulting in 2 hernias from 1 (15,17,18).
Mesh repair has emerged to be superior to primary fascial repair and stoma relocation in terms of recurrence rates with acceptable morbidity risks. The differing techniques of the onlay, retromuscular sublay as well as the intraperitoneal onlay mesh (IPOM) techniques has reported risks of recurrence ranging between 2.1–39% (16,17,19). IPOM techniques, including the Sugarbaker and keyhole methods, have documented superior outcomes of reduced recurrence, lower mesh contamination, haematoma and seroma formation whilst avoiding extensive abdominal wall fascial dissection (20,21). We have opted for a Sugarbaker repair in our case given the comparatively similar recurrence rates without having to create a mesh opening. The alternative keyhole method also has the potential of obstruction from an inadequately sized hernia mesh aperture and is deemed unsuitable in the repair of ileostomies as small bowel can easily herniate through the mesh opening. A biological mesh was applied in this setting of a herniated inflamed gallbladder to further reduce the chances of mesh contamination. There is currently insufficient evidence in promoting the superiority of biological over synthetic meshes under contaminated conditions. While studies have shown no difference in surgical site infections and recurrence rates between the types of meshes, the cases are often not comparable due to differences in mesh placement techniques and short follow up duration (22). This case series is limited in its promotion of one technique over the other due to the small number of cases described. It has, however, provided a basis of comparison between the varying techniques and their outcomes which offers insight into future care and management. Further prospective studies are required to compare the utility of synthetic versus biological meshes.
Given the rarity of gallbladder parastomal herniation, optimal treatment requires careful consideration even as existing reports suggest surgical intervention confers benefit without significant detrimental risks. Perhaps further exploration in the prevention of parastomal hernias in the first place, may be key in circumventing its complications. Until then, any benefit reaped from surgery has to be weighed against a myriad of patient and surgical factors including their potential complications.
Conclusions
Parastomal herniation of the gallbladder and its complications, remains an uncommon presentation that requires further evaluation. An aggressive surgical approach may be used with appropriate case selection and acceptable morbidity and mortality risks.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/dmr-20-82
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr-20-82). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s legal guardian. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Carne PW, Robertson GM, Frizelle FA. Parastomal hernia. Br J Surg 2003;90:784-93. [Crossref] [PubMed]
- Hansson BM, Bleichrodt RP, De Hingh IH. Laparoscopic parastomal hernia repair using a keyhole technique results in a high recurrence rate. Surg Endosc 2009;23:1456-9. [Crossref] [PubMed]
- Cheung MT, Chia NH, Chiu WY. Surgical treatment of parastomal hernia complicating sigmoid colostomies. Dis Colon Rectum 2001;44:266-70. [Crossref] [PubMed]
- St Peter SD, Heppell J. Surgical images: soft tissue. Incarcerated gallbladder in a parastomal hernia. Can J Surg 2005;48:46. [PubMed]
- Garcia RM, Brody F, Miller J, et al. Parastomal herniation of the gallbladder. Hernia 2005;9:397-9. [Crossref] [PubMed]
- Rashid M, Abayasekara K, Mitchell E. A case report of an incarcerated gallbladder in a parastomal hernia. Int J Surg 2010;23:8.
- Rosenblum JK, Dym RJ, Sas N, et al. Gallbladder torsion resulting in gangrenous cholecystitis within a parastomal hernia: findings on unenhanced CT. J Radiol Case Rep 2013;7:21. [Crossref] [PubMed]
- To H, Brough S, Pande G. Case report and operative management of gallbladder herniation. BMC Surg 2015;15:72. [Crossref] [PubMed]
- Gomez-Artacho M, Boisset G, Taoum C, et al. Complicated parastomal hernia as a clinical presentation of a gallbladder hydrops. Cir Esp 2017;95:347. [Crossref] [PubMed]
- Frankl J, Michailidou M, Maegawa F. Parastomal gallbladder hernia in a septic patient. Radiol Case Rep 2017;12:508-10. [Crossref] [PubMed]
- Bakshi C, Ruff S, Caliendo F, et al. Acute cholecystitis in a parastomal hernia causing a small bowel obstruction. J Surg Case Rep 2017;2017:rjx235. [Crossref] [PubMed]
- Brown RA, Kann B, Woolridge J. Parastomal hernia with incarcerated gallbladder: a case report. Int J Surg Res Pract 2018. doi:
10.23937/2378-3397/1410072 . - Rogers P, Lai A, Salama P. Gallbladder complicating a parastomal hernia. J Surg Case Rep 2019;2019:rjz107. [Crossref] [PubMed]
- Hansson BM, Slater NJ, van der Velden AS, et al. Surgical techniques for parastomal hernia repair: a systematic review of the literature. Ann Surg 2012;255:685-95. [Crossref] [PubMed]
- Rieger N, Moore J, Hewett P, et al. Parastomal hernia repair. Colorectal Dis 2004;6:203-5. [Crossref] [PubMed]
- Ripoche J, Basurko C, Fabbro-Perray P, et al. Parastomal hernia. A study of the French federation of ostomy patients. J Visc Surg 2011;148:e435-41. [Crossref] [PubMed]
- Helgstrand F, Rosenberg J, Kehlet H, et al. Risk of morbidity, mortality, and recurrence after parastomal hernia repair: a nationwide study. Dis Colon Rectum 2013;56:1265-72. [Crossref] [PubMed]
- Steele SR, Lee P, Martin MJ, et al. Is parastomal hernia repair with polypropylene mesh safe? Am J Surg 2003;185:436-40. [Crossref] [PubMed]
- Hansson BM, Morales-Conde S, Mussack T, et al. The laparoscopic modified Sugarbaker technique is safe and has a low recurrence rate: a multicenter cohort study. Surg Endosc 2013;27:494-500. [Crossref] [PubMed]
- Gameza VA, Bell Lybecker M, Wara P. Laparoscopic Keyhole Versus Sugarbaker Repair in Parastomal Hernia: A Long-Term Case-Controlled Prospective Study of Consecutive Patients. J Laparoendosc Adv Surg Tech A 2020;30:783-9. [Crossref] [PubMed]
- Funayama Y, Takahashi KI, Ikezawa F, et al. Parastomal hernia repair with the Sugarbaker technique using e-PTFE mesh. Surg Today 2016;46:62-5. [Crossref] [PubMed]
- Primus FE, Harris HW. A critical review of biologic mesh use in ventral hernia repairs under contaminated conditions. Hernia 2013;17:21-30. [Crossref] [PubMed]
Cite this article as: Guo Y, Lye TJY, Lee ZJ, Lim EKW. Gallbladder herniation and cholecystitis within a parastomal hernia: a case report and literature review. Dig Med Res 2020;3:73.



