经肛门全直肠系膜切除术的肿瘤学疗效
前言
全直肠系膜切除术(TME)已成为直肠癌根治手术的金标准技术[1]。环周切缘(CRM)、远端切缘(DRM)和TME质量是直接影响局部复发(LR)和肿瘤特异性生存率的主要组织病理学指标[2]。
技术和手术创新的优势导致了微创技术的引入,包括腹腔镜、机器人和最近的经肛门TME(TaTME)。
肥胖男性的中低位直肠癌患者是直肠低位前切除术的一个众所周知的难点,尤其是腹腔镜TME的手术。有人担心,这些具有狭窄、放射状骨盆和肥大的直肠系膜的病人在接受保留括约肌的切除术中,可能会有环周切缘阳性,或者低质量的TME,甚至是不必要的腹会阴联合切除术(APR)。TaTME的概念已被提出,以克服在这些更困难的病例中经腹方法(开放、腹腔镜、机器人)所遇到的技术挑战。
最近的随机对照试验[3-6]和比较研究[7-8]报告了开腹、腹腔镜和机器人不同手术方式的短期和长期肿瘤学疗效是类似的。最近有研究声称,TaTME至少有三个肿瘤学优势。(I)由于在直视下进行远端离断,DRM更长;(II) CRM阳性率更低;(III) TME质量更高。然而,与腹腔镜和机器人TME相比,TaTME的肿瘤学疗效仍有争议。
本综述的目的是评价TaTME的肿瘤学疗效。
方法
在PubMed、MEDLINE和Cochrane Library进行了文献检索,截止2019年8月30日。两位评审员(CF, AL)独立地在电子数据库(PubMed, MEDLINE, Cochrane Library)中使用以下搜索标题进行了搜索。("laparoscopic TME"或"lapTME")和("TaTME")或("robototic rectal surgery"); ("transanal TME"或("taTME") OR ("Transanal Totorectal Excision")。("transanal"或"transanal endoscopic microsurgery")或("transanal minimally invasive surgery")或("natural orifice transluminal endoscopic surgery")或("NOTES")和("Tatme oncological outcomes")。
此外,还对已确定的文章所提供的参考文献进行了手工搜索,以防止搜索策略造成的文章丢失。这种交叉搜索直到没有更多的相关文献被发现。纳入标准是关于直肠癌TaTME的前瞻性、回顾性、随机性、比较性研究。排除标准是:摘要、信件、社论、技术说明、专家意见、综述、荟萃分析、报告良性病变的研究、未明确报告患者结果和参数的研究、无法从已发表的结果中提取适当数据的研究、已发表文献中作者和中心之间的重叠、患者数量(<10)不合适的研究;非英语论文。
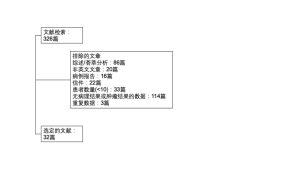
文献检索得到了326篇论文,经过筛选,有32篇文章被选中。该过程见图1。
结果
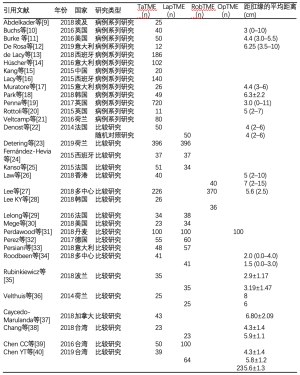
在入选的32篇文章中,13篇是病例系列研究[9-21],19篇是病例对照研究[22-40],其中一篇是随机对照试验[22]。发表时间从2014年[22-36]到2019年[12,23,40]不等。17项研究[10-12,17-20,22,26-28,34-38,40]报告了肿瘤与肛门边缘的平均距离,TaTME组距肛门距离从2[34]到8厘米[36],腹腔镜TME组距肛门距离从1.5[34]到7厘米[26]。详见表1。
Full table
淋巴结检出数量
在31项研究中,有26项研究报告了淋巴结检出平均数,在TaTME组中从10.7[28]到26.45[26];在腹腔镜TME(LapTME)组中从11[28]到26.69[26];在机器人TME(RobTME)组中从13[17]到16.8[18]。1项研究报告了开腹TME(OpTME)手术组平均淋巴结检出数,为23.5±8.2[7]。
在16项比较研究中,有一项[31]报告了经肛和开腹TME(OpTME)在淋巴结检出数量上的统计学差异,但在比较经肛和腹腔镜TME(LapTME)时没有统计学差异。详见表2。
Full table
远端切缘(DRM)
在31项研究中,有25项[9-15,17-20,22,24-28,31-34,36,38-40]报告了TaTME的DRM,范围从1厘米[3,10,14,29]到2.8厘米[24]。10项研究[22,24,25,31,33-36,38-40]报告了腹腔镜手术后DRM的平均长度,范围从1厘米[10]到2.5厘米[36]。4篇[26-28,32]文章报告了RobTME手术后DRM的平均长度,范围从1.5厘米[27]到3.1厘米[32]。2项研究[31,40]报告了OpTME手术后的DRM,范围从1.6厘米到3.47厘米。
在18项[24,31-33,39]比较研究中,有5项[6,25,27,31,32]报告了DRM平均长度上有显著的统计学差异。三项研究报告了TaTME与LapTME相比,DRM的平均长度显著加长[6,25,27]。一项研究[32]报告了RobTME与TaTME相比,DRM更长。Perdawood等人[31]报告了TaTME或LapTME与OpTME相比,DRM更长,但TaTME与LapTME之间没有统计学差异。六项比较研究[22,25,27,30,31,34]报告了TaTME和LapTME病例的DRM阳性率,从0%到8%不等,在唯一报告RobTME的研究中DRM阳性率为0.3%[27]。各项研究中在DRM阳性率方面均无统计学差异。详见表2。
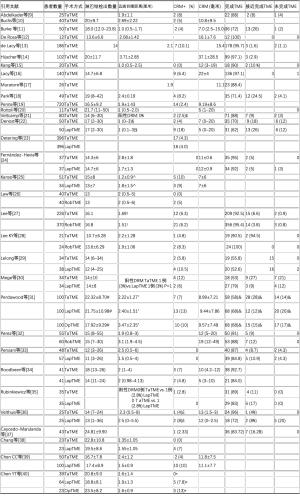
环周切缘(CRM)
27项研究报告了TaTME手术后的CRM阳性的情况(表2)。TaTME术后CRM阳性率从0%[15,24,26,33,38,40]到12%[30]不等,7项研究[22-25,29-31]报告LapTME术后CRM阳性率从0%[24,33,35]到13%[31],3项研究[26-28]报告RobTME术后CRM阳性率从5%[26]到8.3%[28],两项研究[31,40]报告OpTME术后CRM阳性率为10%和13%。三项研究[22,38,40]报告了TaTME对比LapTME或OpTME[40]的CRM阳性率显著降低。在这3项研究[22,38,40]中,有一项是RCT研究[22],比较了经肛门和腹腔镜的手术方法。25项研究[9-11,13,15,16,18,19,22-31,33-35,37-40]中定义阳性CRM的范围为1毫米,2项研究[21,36]为2毫米。18项研究[10-17,19,20,22,24,25,31,32,34,36,39]报告了CRM的宽度(毫米),其中8项是比较性研究[22,24,25,31,32,34,36,39]。TaTME的CRM宽度从5毫米[20]到37.1毫米[14]不等,LapTME从5[22,34]到12毫米[24,36]。有一项研究报告了OpTME[31]和RobTME[32]中CRM的宽度。后者[32]报告了RobTME与TaTME组相比,CRM的宽度之间比较具有统计学差异。详见表2。
TME的质量
根据Quirke[41]的标准对23项研究[9,11-18,21,22,24,27-37](其中12项比较研究[22,24,27-36])的TME的质量进行评估。达到TME完整切除的手术在TaTME的占比从53%[30]到100%[12]不等,在评估LapTME的9项研究[22,24,29-31,33-37]中从52.6%[29]到92%[24]不等,在报告RobTME的3项研究[27,28,32]中从88%[32]到100%[28]不等,在报告OpTME的一项研究中为68%[31]。未达到TME完整切除的手术,在TaTME中的占比从0%[12,15,20,24,28,29,32,35-37]到21%[30],在LapTME中从0%[28,35]到20%[31,36],在2项报告RobTME的研究中为0%[28,32],在一项报告OpTME的研究中为17%[31]。在12项比较研究[22,24,27-36]中,有两项研究[31,36]报告TaTME与LapTME相比,达到完整TME切除的差异具有统计学意义。详见表2。
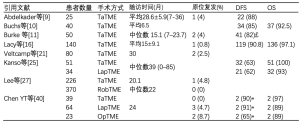
远期生存
有八项研究[9,10,11,16,21,25,27,40]报告了长期随访数据,其中三项是比较研究[25,27,40]。随访时间以中位数(15.1-39个月)[11,25,27]或平均数(15-28.6个月)[9,10,16]报告。TaTME后的局部复发率(LR)、无病生存率(DFS)和总生存率(OS)分别从0%[40]到4.8%[27],从63%[25]到90.8%[16],从92.5%[10]到100%[25]。Chen等人[40]报道,当TaTME和LapTME与OpTME相比,DFS在统计学上更高(P=0.01),当TaTME与LapTME相比,DFS没有差异(P=0.7)。详见表3。
Full table
讨论
中低位直肠癌的治疗金标准是TME,它已被证实可以改善局部清扫率[1]并降低原位复发率[42]。
腹腔镜和机器人TME代表了直肠肿瘤治疗的一个飞跃,提供了更好的短期预后和类似的远期预后[3-8,43]。然而,以高质量的TME进行直肠前部切除在技术上具有挑战性,尤其是通过腹腔镜,因为远端直肠系膜变窄,神经血管束难以辨认,尤其是因为手术视野有限,导致腹腔镜下器械难以看到,难以在骨盆深部放置和移动吻合器。上述因素与不理想的吻合技术相结合,会导致远端切缘不够、直肠系膜不完整和环周切缘受累,从而导致局部复发。以前的RCT研究[3,44]发现腹腔镜TME的环周切缘(CRM)阳性率很高(7%~12.1%)。ROLARR试验[8]发现RobTME比LapTME在统计学上没有明显的肿瘤学或临床优势,CRM阳性率分别为5.1%和6.3%。TaTME的"自下而上"的方法是为了尽量减少 "自上而下"的限制而开创的。事实上,TaTME有助于清楚地暴露解剖平面,准确地确定狭窄盆腔的切除边缘,以及更直接地处理直肠远端解剖,从而产生更好的围手术期结果,提高肿瘤学质量,以及更好的神经保护[45,46]。
本文就TME的质量做出综述, DRM和CRM被认为是衡量TME质量的标准,还是影响直肠前切除术后原位复发率和生存率的主要预后因素[1,41,47]。与经腹手术(腹腔镜、机器人、开腹)相比,TaTME提供了良好的肿瘤学疗效,也可能获得了更低的CRM阳性率和TME不完整率。最近的两项荟萃分析也报告了类似的结果,一个比较了Ta-和LapTME[48]和另一个比较了Ta-、Rob-和OpTME[49]。Ma等人[50]在他们的系统回顾和荟萃分析中报告了TaTME与LapTME相比,CRM更长,CRM阳性率更低,完整TME切除率更高。另一项分析Ta-和RobTME的荟萃分析[51]报告,TaTME手术的CRM阳性率更低,尽管这一结果在统计学上和临床上都没有意义。另外,一项RCT研究[22]比较了Ta-和LapTME,报告了“自下而上”的手术方法的CRM阳性率有显著降低。
不可否认的是,TaTME的核心价值在直视下完成直肠横断以实现足够的肿瘤远端切缘。然而,正如最近的荟萃分析[51]所报告的那样,各研究在远端切缘方面没有明显差异。令人惊讶的是,一项研究[32]报告说,与机器人方法相比,TaTME组的远端切缘和环周切缘长度更低,尽管两组在肿瘤大小和部位、新辅助治疗或Quirke分级方面没有差异。然而,对标本进行不同的病理评估可能存在不同机构间的差异,从而影响了结果。由于这个原因,与DRM有关的结果应谨慎解释,必须指出已发表的研究在肿瘤大小和肿瘤分期方面的差异,最主要的是肿瘤位置的差异[48,50,51]。
Perdawood等人[52]的研究旨在比较29例TaTME和29例LapTME的术后手术样本的缺损,报告了TaTME组的DRM明显更长(33.45+14.5 vs. 25.41+11.16;P=0.048)。有趣的是,TaTME组中腹膜反射以下的手术标本的缺损比例明显较低,这表明TaTME有可能通过改善直肠下端的分离来改善直肠癌手术。
值得注意的是,大多数研究的结果和外科医生的学习曲线也有一定的关系,尽管如此,结果还是非常有希望的。
大多数研究只报告了短期结果,这也反映了TaTME的创新性。这种新方法是否在LR、DFS和癌症特异性生存方面具有类似的肿瘤学结果,需要在前瞻性试验中进一步研究,将TaTME与腹腔镜或机器人TME在更长的随访时间后进行比较。
随着TaTME的术式被越来越多的外科医生采用,患者的选择也将是继续引发讨论的关键因素。希望具有严格入组标准的国际性TaTME的临床研究如COLOR III前瞻性随机对照研究[53]能对TaTME(与腹腔镜)后的短期和长期肿瘤学疗效给出明确的答案。
总结
TaTME是一种肿瘤学上安全和有效的技术,与经腹手术方法相比,至少能产生类似的肿瘤学疗效。为了进一步明确TaTME在直肠癌治疗中的作用,需要实现手术技术的标准化、常规手术的可操作性,以及严格的患者选择标准。希望COLOR III多中心RCTs将阐明TaTME后的短期和远期肿瘤学疗效。
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Janindra Warusavitarne and Roel Hompes) for the series “TaTME” published in Digestive Medicine Research. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2019.12.01). The series “TaTME” was commissioned by the editorial office without any funding or sponsorship. AS acted as teacher/consultant/speaker for Ethicon and Takeda. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery: the clue to pelvic recurrence? Br J Surg 1982;69:613-6. [Crossref] [PubMed]
- Birbeck KF, Macklin CP, Tiffin NJ, et al. Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg 2002;235:449-57. [Crossref] [PubMed]
- van der Pas MH, Haglind E, Cuesta MA, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 2013;14:210-8. [Crossref] [PubMed]
- Jeong SY, Park JW, Nam BH, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 2014;15:767-74. [Crossref] [PubMed]
- Kang SB, Park JW, Jeong SY, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 2010;11:637-45. [Crossref] [PubMed]
- Jayne DG, Thorpe HC, Copeland J, et al. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 2010;97:1638-45. [Crossref] [PubMed]
- Park EJ, Cho MS, Baek SJ, et al. Long-term oncologic outcomes of robotic low anterior resection for rectal cancer: a comparative study with laparoscopic surgery. Ann Surg 2015;261:129-37. [Crossref] [PubMed]
- Jayne D, Pigazzi A, Marshall H, et al. Robotic-assisted surgery compared with laparoscopic resection surgery for rectal cancer: the ROLARR RCT. Efficacy and Mechanism Evaluation 2019. doi:
10.3310/eme06100 . - Abdelkader AM, Zidan AM, Younis MT, et al. Transanal total mesorectal excision for the treatment of carcinoma in the Middle or Lower Third Rectum: the Technical Feasibility of the Procedure, Pathological Results, and Clinical Outcome. Indian J Surg Oncol 2018;9:442-51. [Crossref] [PubMed]
- Buchs NC, Wynn G, Austin R, et al. A two-centre experience of transanal total mesorectal excision. Colorectal Dis 2016;18:1154-61. [Crossref] [PubMed]
- Burke JP, Martin-Perez B, Khan A, et al. Transanal total mesorectal excision for rectal cancer: early outcomes in 50 consecutive patients. Colorectal Dis 2016;18:570-7. [Crossref] [PubMed]
- De Rosa M, Rondelli F, Boni M, et al. Transanal total mesorectal excision (TaTME): single-centre early experience in a selected population. Updates Surg 2019;71:157-63. [Crossref] [PubMed]
- de Lacy FB, van Laarhoven JJEM, Pena R, et al. Transanal total mesorectal excision: pathological results of 186 patients with mid and low rectal cancer. Surg Endosc 2018;32:2442-7. [Crossref] [PubMed]
- Hüscher CG, Tierno SM, Romeo V, et al. Technologies, technical steps, and early postoperative results of transanal TME. Minim Invasive Ther Allied Technol 2016;25:247-56. [Crossref] [PubMed]
- Kang L, Chen WH, Luo SL, et al. Transanal total mesorectal excision for rectal cancer: a preliminary report. Surg Endosc 2016;30:2552-62. [Crossref] [PubMed]
- Lacy AM, Tasende MM, Delgado S, et al. Transanal Total Mesorectal Excision for Rectal Cancer: Outcomes after 140 Patients. J Am Coll Surg 2015;221:415-23. [Crossref] [PubMed]
- Muratore A, Mellano A, Marsanic P, et al. Transanal total mesorectal excision (taTME) for cancer located in the lower rectum: short- and mid-term results. Eur J Surg Oncol 2015;41:478-83. [Crossref] [PubMed]
- Park SC, Sohn DK, Kim MJ, et al. Phase II Clinical Trial to Evaluate the Efficacy of Transanal Endoscopic Total Mesorectal Excision for Rectal Cancer. Dis Colon Rectum 2018;61:554-60. [Crossref] [PubMed]
- Penna M, Hompes R, Arnold S, et al. Transanal Total Mesorectal Excision: International Registry Results of the First 720 Cases. Ann Surg 2017;266:111-7. [Crossref] [PubMed]
- Rottoli M, Hanna L, Kukreja N, et al. Is transanal total mesorectal excision a reproducible and oncologically adequate technique? A pilot study in a single center. Int J Colorectal Dis 2016;31:359-63. [Crossref] [PubMed]
- Veltcamp Helbach M, Deijen CL, Velthuis S, et al. Transanal total mesorectal excision for rectal carcinoma: short-term outcomes and experience after 80 cases. Surg Endosc 2016;30:464-70. [Crossref] [PubMed]
- Denost Q, Adam JP, Rullier A, et al. Perineal transanal approach: a new standard for laparoscopic sphincter-saving resection in low rectal cancer, a randomized trial. Ann Surg 2014;260:993-9. [Crossref] [PubMed]
- Detering R, Roodbeen SX, van Oostendorp SE, et al. Three-Year Nationwide Experience with Transanal Total Mesorectal Excision for Rectal Cancer in the Netherlands: A Propensity Score-Matched Comparison with Conventional Laparoscopic Total Mesorectal Excision. J Am Coll Surg 2019;228:235-44.e1. [Crossref] [PubMed]
- Fernández-Hevia M, Delgado S, Castells A, et al. Transanal total mesorectal excision in rectal cancer: short-term outcomes in comparison with laparoscopic surgery. Ann Surg 2015;261:221-7. [Crossref] [PubMed]
- Kanso F, Maggiori L, Debove C, et al. Perineal or Abdominal Approach First During Intersphincteric Resection for Low Rectal Cancer: Which Is the Best Strategy? Dis Colon Rectum 2015;58:637-44. [Crossref] [PubMed]
- Law WL, Foo DCC. Comparison of early experience of robotic and transanal total mesorectal excision using propensity score matching. Surg Endosc 2019;33:757-63. [Crossref] [PubMed]
- Lee L, de Lacy B, Gomez Ruiz M, et al. A Multicenter Matched Comparison of Transanal and Robotic Total Mesorectal Excision for Mid and Low-rectal Adenocarcinoma. Ann Surg 2019;270:1110-6. [Crossref] [PubMed]
- Lee KY, Shin JK, Park YA, et al. Transanal Endoscopic and Transabdominal Robotic Total Mesorectal Excision for Mid-to-Low Rectal Cancer: Comparison of Short-term Postoperative and Oncologic Outcomes by Using a Case-Matched Analysis. Ann Coloproctol 2018;34:29-35. [Crossref] [PubMed]
- Lelong B, Meillat H, Zemmour C, et al. Short- and Mid-Term Outcomes after Endoscopic Transanal or Laparoscopic Transabdominal Total Mesorectal Excision for Low Rectal Cancer: A Single Institutional Case-Control Study. J Am Coll Surg 2017;224:917-25. [Crossref] [PubMed]
- Mege D, Hain E, Lakkis Z, et al. Is trans-anal total mesorectal excision really safe and better than laparoscopic total mesorectal excision with a perineal approach first in patients with low rectal cancer? A learning curve with case-matched study in 68 patients. Colorectal Dis 2018;20:O143-51. [Crossref] [PubMed]
- Perdawood SK, Thinggaard BS, Bjoern MX. Effect of transanal total mesorectal excision for rectal cancer: comparison of short-term outcomes with laparoscopic and oper surgeries. Surg Endosc 2018;32:2312-21. [Crossref] [PubMed]
- Perez D, Melling N, Biebl M, et al. Robotic low anterior resection versus transanal total mesorectal excision in rectal cancer: A comparison of 115 cases. Eur J Surg Oncol 2018;44:237-42. [Crossref] [PubMed]
- Persiani R, Biondi A, Pennestrì F, et al. Transanal Total Mesorectal Excision vs Laparoscopic Total Mesorectal Excision in the Treatment of Low and Middle Rectal Cancer: A Propensity Score Matching Analysis. Dis Colon Rectum 2018;61:809-16. [Crossref] [PubMed]
- Roodbeen SX, Penna M, Mackenzie H, et al. Transanal total mesorectal excision (TaTME) versus laparoscopic TME for MRI-defined low rectal cancer: a propensity score-matched analysis of oncological outcomes. Surg Endosc 2019;33:2459-67. [Crossref] [PubMed]
- Rubinkiewicz M, Nowakowski M, Wierdak M, et al. Transanal total mesorectal excision for low rectal cancer: a case-matched study comparing TaTME versus standard laparoscopic TME. Cancer Manag Res 2018;10:5239-45. [Crossref] [PubMed]
- Velthuis S, Nieuwenhuis DH, Ruijter TE, et al. Transanal versus traditional laparoscopic total mesorectal excision for rectal carcinoma. Surg Endosc 2014;28:3494-9. [Crossref] [PubMed]
- Caycedo-Marulanda A, Ma G, Jiang HY. Transanal total mesorectal excision (taTME) in a single-surgeon setting: refinements of the technique during the learning phase. Tech Coloproctol 2018;22:433-43. [Crossref] [PubMed]
- Chang TC, Kiu KT. Transanal Total Mesorectal Excision in Lower Rectal Cancer: Comparison of Short-Term Outcomes with Conventional Laparoscopic Total Mesorectal Excision. J Laparoendosc Adv Surg Tech A 2018;28:365-9. [Crossref] [PubMed]
- Chen CC, Lai YL, Jiang JK, et al. Transanal Total Mesorectal Excision Versus Laparoscopic Surgery for Rectal Cancer Receiving Neoadjuvant Chemoradiation: A Matched Case-Control Study. Ann Surg Oncol 2016;23:1169-76. [Crossref] [PubMed]
- Chen YT, Kiu KT, Yen MH, et al. Comparison of the short-term outcomes in lower rectal cancer using three different surgical techniques: Transanal total mesorectal excision (TME), laparoscopic TME, and open TME. Asian J Surg 2019;42:674-80. [Crossref] [PubMed]
- Quirke P, Steele R, Monson J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet 2009;373:821-8. [Crossref] [PubMed]
- van Gijn W, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 2011;12:575-82. [Crossref] [PubMed]
- Bonjer HJ, Deijen CL, Abis GA, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 2015;372:1324-32. [Crossref] [PubMed]
- Fleshman J, Branda M, Sargent DJ, et al. Effect of laparoscopic assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 2015;314:1346-55. [Crossref] [PubMed]
- Heald RJ. A new solution to some old problems: transanal TME. Tech Coloproctol 2013;17:257-8. [Crossref] [PubMed]
- Aigner F, Hörmann R, Fritsch H, et al. Anatomical considerations for transanal minimal-invasive surgery: the caudal to cephalic approach. Colorectal Dis 2015;17:O47-53. [Crossref] [PubMed]
- Nagtegaal ID, van de Velde CJ, van der Worp E, et al. Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 2002;20:1729-34. [Crossref] [PubMed]
- Zhang X, Gao Y, Dai X, et al. Short- and long-term outcomes of transanal versus laparoscopic total mesorectal excision for mid-to-low rectal cancer: a meta-analysis. Surg Endosc 2019;33:972-85. [Crossref] [PubMed]
- Simillis C, Lal N, Thoukididou SN, et al. Open versus laparoscopic versus robotic versus transanal mesorectal excision for rectal cancer. A systematic review and network meta-analysis. Ann Surg 2019;270:59-68. [Crossref] [PubMed]
- Ma B, Gao P, Song Y, et al. Transanal total mesorectal excision (TaTME) for rectal cancer: a systematic review and meta-analysis of oncological and perioperative outcomes compared with laparoscopic total mesorectal excision. BMC Cancer 2016;16:380. [Crossref] [PubMed]
- Gachabayov M, Tulina I, Bergamaschi R, et al. Does transanal mesorectal excision of rectal cancer improvce histopathology metrics and/or complication rates? A meta analysis. Surg Oncol 2019;30:47-51. [Crossref] [PubMed]
- Perdawood SK, Warnecke M, Bjoern MX, et al. The pattern of defects in mesorectal specimens: is there a difference between transanal and laparoscopic approaches? Scand J Surg 2019;108:49-54. [Crossref] [PubMed]
- Deijen CL, Velthuis S, Tsai A, et al. COLOR III: a multicenter randomised clinical trial comparing transanal TME versus laparoscopic TME for mid and low rectal cancer. Surg Endosc 2016;30:3210-5. [Crossref] [PubMed]

冯雯卿
医学博士,上海交通大学医学院附属瑞金医院普外科博士后,毕业于上海交通大学医学院临床医学八年制专业, 2020年至今工作于上海交通大学医学院附属瑞金医院普外科博士后工作站,从事结直肠肿瘤以及肿瘤免疫微环境相关研究。(更新时间:2021/9/5)
(本译文仅供学术交流,实际内容请以英文原文为准。)
Cite this article as: Foppa C, Luberto A, Spinelli A. Oncological outcomes for transanal total mesorectal excision. Dig Med Res 2020;3:17.