
Symptomatic annular pancreas in an adult: an unusual cause of abdominal pain
Introduction
Annular pancreas is a rare congenital disorder that results from the failure of the ventral bud to rotate with the duodenum during the 7th week of gestation to fuse with the dorsal bud, resulting in a ring of pancreatic parenchyma that surrounds the second portion of the duodenum, and it usually presents in newborns and infants (1). The onset of presentation depends on the severity of the duodenal constriction. When the constriction is severe enough to cause obstruction it usually presents itself in newborns and infants with symptoms of gastric outlet obstruction, and is associated with other congenital abnormalities as Down syndrome and other intestinal anomalies (2). When the envelopment doesn’t result in duodenal obstruction, it usually passes unnoticed. It is estimated that approximately two-thirds of the cases remain asymptomatic for life, and when symptomatic it is rarely diagnosed due to the mild nature of the symptoms. We present a case of an annular pancreas in an adult that developed severe symptoms that required surgical management.
Case presentation
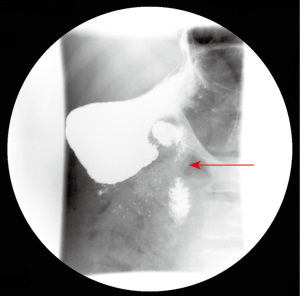
A 46-year-old Caucasian male with a smoking index of 30 pack-years and chronic alcohol consumption of 160 grams per day, with no history of past medical conditions, and with a family history of pancreatic and gastric cancer, presented to the emergency unit with a 6-month history of intermittent colicky epigastric pain irradiated to both hypochondria and back, with a progressive increase in intensity that worsened with food intake causing a limitation to food ingestion that lead to asthenia and loss of 20 kg. of weight in the previous 6 months. He also described post-prandial fullness, nausea and a change in bowel habits for the last 5 months in the form of progressive constipation for which he underwent colonoscopy 3 months prior to his presentation that only revealed a sessile polyp in the descending colon without histological abnormalities. He denied vomiting, hematemesis, hematochezia or melena. On examination he was normotensive, afebrile, with normal rubor. Abdominal examination revealed tenderness in epigastrium and both hypochondria with abdominal guarding, and normal bowel sounds. No masses were palpated. Proton pump inhibitors, gastroprokinetic agents and analgesia with acetaminophen and metamizole didn’t alleviate his symptoms. Laboratory tests revealed normal leukocyte count, acute phase reactants, liver and pancreatic enzymes. Abdominal X-ray showed no abnormalities, and he was admitted to hospital for further study, undergoing upper gastrointestinal endoscopy that revealed grade I oesophageal varices, mild hiatal hernia and chronic antral gastropathy. Abdominal ultrasonography revealed a small hepatic hemangioma with homogenous hepatic parenchyma, and no biliary, pancreatic or splenic anomalies. After progression of the severity of symptoms further study was followed with computerized tomographic enterography that revealed a band of pancreatic parenchyma surrounding the descending portion of the duodenum, with the pancreatic duct opening in the duodenum anterior and superior to the biliary duct opening (Figure 1). Barium meal was done that revealed an extrinsic compressing effect on the descending part of the duodenum without obstruction, proximal dilatation or gastric retention (Figure 2). Conservative treatment with analgesics, soft diet, proton pump inhibitors and gastroprokinetic agents was decided at first considering that the patient didn’t show duodenal obstruction or any other complication, with failure to control the symptoms. Due to failure of conservative treatment and high risk of the patient to develop complications (chronic smoker and heavy alcohol consumer, family history) surgical approach was decided. Laparoscopic duodenojejunostomy was performed with no post-operative complications. No enlarged lymph nodes were detected in the periportal or peripancreatic regions. Relief of symptoms was achieved after 48 hours of the procedure. The patient had an improved appetite with progressive gain of weight in the following year of follow-up.

Discussion
The first report of this congenital anomaly was done by Tiedemann in 1818, and was given the name “annular pancreas” by Ecker in 1862. Drey classified it according to age of presentation into neonatal, pediatric, adult asymptomatic and adult symptomatic annular pancreas (3). The precise prevalence is unclear as most patients are asymptomatic and are not diagnosed, and wh;;;en symptomatic it usually passes unnoticed and misdiagnosed due to the mild nature of the symptoms in most cases. In autopsy series the prevalence ranges from 5 to 15 per 100,000 adults (4-6).
The most common symptoms in adult patients with annular pancreas are cramping epigastric pain, postprandial fullness and relief with vomiting. The most common complications are peptic ulceration, upper gastrointestinal bleeding, and pancreatitis and may lead to duodenal obstruction due to chronic inflammation and fibrosis of the pancreatic annulus (7). There have been recently two case reports associating intraduct papillary mucinous neoplasm on biopsy after resection (8,9). It has been rarely related with obstructive jaundice (10), and some case reports suggest that when this occurs it is due to an underlying periampullary neoplasm (11). CT and MR are the most appropriate imaging modalities to evaluate pancreatoduodenal junction (12); and it can be diagnosed without the finding of a radiological complete ring of pancreatic tissue (13). It can also be diagnosed by using endoscopic ultrasound (14).
Surgery is the treatment of choice in patients with symptoms that can be attributed to the annular pancreas, with the aim of relieving the duodenal or gastric outlet obstruction by bypassing the annulus. The resection of the annulus is not recommended as it has been associated with pancreatic fistulae, pancreatitis, and incomplete relief of duodenal obstruction (2). Most adult patients are asymptomatic or have mild symptoms that only require conservative medical treatment. Surgical management is reportedly indicated when these complications become severe or frequent. We present a case of severely symptomatic annular pancreas in an adult that showed no duodenal obstruction and surgical management was decided despite the absence of the previously mentioned complication, with good results and relief of symptoms.
The surgical procedure of choice in adults is gastrojejunostomy or duodenojejunostomy (15), while in neonates duodenoduodenostomy is preferred as the duodenum is more mobile. Pancreaticoduodenectomy is recommended when annular pancreas presents as obstructive jaundice due to chronic pancreatitis or periampullary lesions suspicious for neoplasm (10,11).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2019.03.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). The patient gave his consent for the publication of the case description and images. We obtained the approval from our hospital’s Ethics Committee to use the clinical data of this case for subsequent publication.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Etienne D, John A, Menias CO, et al. Annular pancreas: a review of its molecular embryology, genetic basis and clinical considerations. Ann Anat 2012;194:422-8. [Crossref] [PubMed]
- Sencan A, Mir E, Günsar C, et al. Symptomatic annular pancreas in newborns. Med Sci Monit 2002;8:CR434-7. [PubMed]
- DREY NW. Symptomatic annular pancreas in the adult. Ann Intern Med 1957;46:750-72. [Crossref] [PubMed]
- Ravitch MM. The pancreas in infants and children. Surg Clin North Am 1975;55:377-85. [Crossref] [PubMed]
- THEODORIDES T. Annular Pancreas. J Chir (Paris) 1964;87:445-62. [PubMed]
- RAVITCH MM. WOODS AC Jr. Annular pancreas. Ann Surg 1950;132:1116-27. [Crossref]
- Urayama S, Kozarek R, Ball T, et al. Presentation and treatment of annular pancreas in an adult population. Am J Gastroenterol 1995;90:995-9. [PubMed]
- Kobayashi S, Kamohara Y, Nagata Y, et al. Intraductal papillary mucinous neoplasm in an annular pancreas: a case report. Surg Case Rep 2015;1:68. [Crossref] [PubMed]
- Ji FJ, Tian XF, Wei L, et al. A case of annular pancreas accompanied with intraductal papillary mucinous neoplasm-case report. Int J Clin Exp Med 2015;8:3332-7. [PubMed]
- Benger JR, Thompson MH. Annular pancreas and obstructive jaundice. Am J Gastroenterol 1997;92:713-4. [PubMed]
- Shan YS, Sy ED, Lin PW. Annular pancreas with obstructive jaundice: beware of underlying neoplasm. Pancreas 2002;25:314-6. [Crossref] [PubMed]
- Hernandez-Jover D, Pernas JC, Gonzalez-Ceballos S, et al. Pancreatoduodenal junction: review of anatomy and pathologic conditions. J Gastrointest Surg 2011;15:1269-81. [Crossref] [PubMed]
- Sandrasegaran K, Patel A, Fogel EL, et al. Annular pancreas in adults. AJR Am J Roentgenol 2009;193:455-60. [Crossref] [PubMed]
- Kalaitzakis E, Thorlacius H. Portal Annular Pancreas With Retroportal Pancreatic Duct Diagnosed With Endoscopic Ultrasound. Clin Gastroenterol Hepatol 2015;13:e175-6. [Crossref] [PubMed]
- Zilberstein B, Sorbello MP, Orso IR, et al. Laparoscopic duodenal-jejunal bypass for the treatment of duodenal obstruction caused by annular pancreas: description of a surgical technique. Surg Laparosc Endosc Percutan Tech 2011;21:e60-4. [Crossref] [PubMed]
Cite this article as: Shabaka A, Mateos-Sánchez P, Amador-Borrero B, Antolín J, Cigüenza R. Symptomatic annular pancreas in an adult: an unusual cause of abdominal pain. Dig Med Res 2019;2:3.


