Major abdominal surgery in a patient with a metallic heart valve—balancing risks of thromboembolic events and perioperative bleeding
Introduction
Patient is an 83-year-old female who was referred to our institution for management of a supratherapeutic international normalized ratio (INR), rectal bleeding, and generalized weakness. Patient takes Coumadin for prevention of thrombosis from her mechanical mitral valve. Past medical history included atrial fibrillation, hypothyroidism, congestive heart failure, chronic obstructive pulmonary disease, cerebral vascular accident three times over the past 3 years, and mitral valve prolapse with valve replacement. The metallic valve was placed about 8 years prior. Patient was a prior smoker.
Upon physical exam patient had stable vital signs. Patient had an unremarkable physical exam. Admission labs showed severe acute blood loss anemia, with hemoglobin and hematocrit of 6.8 g/dL and 21.6%, respectively. Patient had supratherapeutic INR of 12 and hypoalbuminemia of 2.8 g/dL.
Based on presentation, patient was admitted to the medical service into the intermediate intensive care unit and transfused two units of packed red blood cells (PRBC) and given prothrombin complex concentrate (PCC) along with vitamin K. Gastroenterology (GI) consult was obtained, recommended colonoscopy and endoscopic gastroduodenoscopy (EGD) to locate source of enteral bleeding. Cardiology urged that patent remain anticoagulated, allowing cessation of anticoagulation 6–8 hours prior to procedures, despite symptomatic anemia.
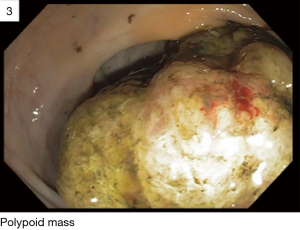
EGD performed by GI was unremarkable. Colonoscopy showed a friable, multilobulated 5 cm polypoid mass at the level of the ileocecal valve, which involved 75% of the mucosal perimeter (Figure 1). Biopsies were taken and proved the mass to be a well-differentiated invasive colonic adenocarcinoma. The medical team performed a metastatic workup and consulted general surgery for resection.
Cardiology cleared patient as moderate risk for procedure, recommending that patient cannot be off anticoagulation for more than 24 hours perioperatively.
On hospital day 7, patient was taken to the operating room for a right hemicolectomy. Intraoperatively, no carcinomatosis or liver/omental masses were found. Adequate hemostasis was achieved and an estimated 75 cc blood loss. Jackson-Pratt (JP) drain was left at site of reanastomosis. Due to prolonged paralytic effect, patient remained intubated and was transferred to the surgical intensive care unit (SICU) for further management.
Continuous heparin infusion was restarted about 12–16 hours postoperatively without any bolus. Goal partial prothrombin time (PTT) was 50–70 seconds for adequate anticoagulation without supratherapeutic effects.
Throughout postoperative hospital course patient had sanguinous fluid drainage from JP drain, with up to 300–400 cc/day. Patient required multiple blood transfusions with PRBC, to which her hemoglobin and hematocrit responded appropriately. It is important to note that the patient’s hemoglobin and hematocrit decreased shortly after supratherapeutic spikes of PTT. Patient was on continuous heparin infusion for about 2 weeks postoperatively.
Discussion
It is well known that mechanical heart valves greatly increase the risk of thromboembolic events. These events can range from complete occlusion of valve to stroke and pulmonary embolisms, causing sever morbidity and mortality. Research has shown that mechanical valves have a much higher incidence of thromboembolism than bioprosthetic valves, causing the need of lifetime anticoagulation. Tricuspid valves are 20 times more likely to develop thrombosis than left sided heart valves; similarly, mitral valves are 2–3 times more likely for thromboembolic events over aortic valves (1).
Currently, there aren’t many studies on the risk versus benefit of anticoagulation in the postoperative period in patients with mechanical valves. Many cardiologists argue that the risk of stopping anticoagulation for greater than 24 hours would outweigh the benefit of preventing postoperative bleeding, stating the risk of nonobstructive thromboembolism in the postoperative period to be as high as 10% (2).
Panduranga et al. stated that there is a 1.8% per patient year risk in thrombotic event without any anticoagulation in patients with mechanical valve. They calculated that the risk of thrombotic events is 4% per patient year, 2.2% with antiplatelet agent, and <1% with Coumadin. In a meta-analysis, it was concluded that a daily risk of 0.06% is added in stopping anticoagulation. Therefore, short-term interruption of anticoagulation is not as dangerous as presumed. They advised that anticoagulation could safely be held for 7–14 days in patients with intracranial hemorrhage, and 24–48 hours in patients with extracranial hemorrhage. This study was only limited to patients taking Warfarin, and only included spontaneous bleeding as opposed to postoperative hemorrhage (3).
Another study reported holding anticoagulation for 1 to 2 weeks for patients who suffer intracranial hemorrhage (ICH) with mechanical heart valve. Phan et al. recommended holding anticoagulation after ICH a mean of 10 days, however, they reported a mechanical valve thrombosis rate of 3% in 30 days (4).
Timing for resuming anticoagulation after major abdominal surgery seems to vary as no common guidelines exist across multiple disciplines. Currently, only retrospective case series are available to guide our clinical protocols. Optimal timing for resuming anticoagulation still presents a challenge for the surgeon as they continue to weigh the risks and benefits.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2018.06.04). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Roudaut R, Serri K, Lafitte S. thrombosis of prosthetic heart valves: diagnosis and therapeutic considerations. Heart 2007;93:137-42. [Crossref] [PubMed]
- Laplace G, Lafitte S, Labèque JN, et al. Clinical significance of early thrombosis after prosthetic mitral valve replacement. J Am Coll Cardiol 2004;43:1283-90. [Crossref] [PubMed]
- Panduranga P, Al-Mukhaini M, Al-Muslahi M, et al. Management dilemmas in patients with mechanical heart valves and warfarin-induced major bleeding. World J Cardiol 2012;4:54-9. [Crossref] [PubMed]
- Phan TG, Koh M, Wijdicks EF. Safety of discontinuation of anticoagulation in patients with intracranial hemorrhage at high thromboembolic risk. Arch Neurol 2000;57:1710-3. [Crossref] [PubMed]
Cite this article as: Parizh D, Kumar S, Meytes V. Major abdominal surgery in a patient with a metallic heart valve—balancing risks of thromboembolic events and perioperative bleeding. Dig Med Res 2018;1:4.