
Pre-optimisation of the cancer patient
The cancer patient presenting for elective surgery
In 2017, the age-standardised incidence rate for cancer in England was 538.0 per 100,000 females and 655.7 per 100,000 males (1). Nearly half of all patients with cancer in England between 2013–2014 had surgery as part of their primary management of care (2) and this workload spans across all surgical specialties. In each year between 2015–2017, 36% of all cancer diagnoses made in the UK were in patients aged 75 and older (3) and the mortality rate from cancer increases with advancing age (1).
There is a relatively small group of ‘high risk’ surgical patients that represent 80% of all deaths in the perioperative period (4). Patients presenting for oncological surgery are increasingly falling into this category due to an ageing population with medical co-morbidities but also as a consequence of the pathophysiological processes associated with cancer and its treatment. It is common to find that cancer patients are anaemic, malnourished due to reduced appetite and physically deconditioned due to fatigue and a lack of engagement with exercise due to low mood. In addition, neoadjuvant treatments can negatively affect other organ systems including the cardiotoxicity associated with certain chemotherapy drugs (5). This is further emphasised by the finding that patients with oesophagogastric adenocarcinoma were noted to have a significantly reduced anaerobic threshold and peak oxygen delivery after neoadjuvant chemotherapy and illustrates an association with a fall in cardiorespiratory reserve and therefore postoperative complications including death (6).
Oncological surgery is associated with potentially significant complications including mortality and morbidity. It is known that major surgery results in a systemic inflammatory response with an increased requirement for oxygen. Cancer patients often lack the physiological reserve to increase their cardiac output to mitigate the demand placed due to the surgery (7). As expected, it has been shown that postoperative complications in the colorectal surgical subgroup were more likely if the patient was deemed ‘high risk’ with concomitant medical co-morbidities and this is also associated with a significant financial burden (8).
This cohort is distinct from other patients presenting for elective surgery from the perspective that oncological surgery is usually time critical due to the risk of disease progression. There is often a lack of both time and resources in order to address the individual issues that can be optimised pre-operatively with the aim of improving patient outcome and also having a health economic benefit. In this review article, we will address the rationale, evidence and limitations for the multimodal components to the pre-optimisation of the cancer patient.
Pre-optimisation of the cancer patient
Current ethos of pre-optimisation
The Royal College of Anaesthetists in the UK has launched a ‘Fitter, Better, Sooner’ campaign in 2019. There is an online tool that provides information to patients on how to be more engaged with the process of preparing for an operation and how to achieve better outcomes postoperatively through lifestyle choices and optimisation of medical co-morbidities (9). Pre-optimisation is in the forefront of perioperative medicine and this latest publicity highlights the patient-centred approach that needs to be adopted in order to have patients arriving in the anaesthetic room on the day of surgery in the most optimal condition possible.
Pre-operative assessment clinic
The current model of pre-operative assessment in most institutions relies on a specialist nurse-led identification of ‘high risk’ patients who are then referred to an anaesthetist in order to review the patient. Some institutions have a ‘one stop’ pre-assessment clinic setup where an anaesthetist will then refer the patient immediately for further diagnostic tests including echocardiography but also for therapeutic interventions such as a pre-operative iron infusion. The pre-assessment clinic also provides a ‘teachable moment’ to optimise patients including promotion of exercise, adoption of a healthier diet, reduction in alcohol intake and offering smoking cessation advice if applicable. There has also been a shift in the ethos from paternalistic to shared decision-making (10). Scoring tools can be used in the pre-operative assessment clinic to convey the individual patient’s risk of mortality and perioperative complications. This is essential as the information provided enables the patient to give their consent to surgery and assists in managing patient expectations in the perioperative period. Alternatively, if the patient does not consent to the surgery based on the perceived risk and benefit, this provides an opportunity to discuss alternatives in treatment.
Many institutions specialising in oncological surgery are part of evidence-based and focused Enhanced Recovery After Surgery (ERAS) programmes. These are modelled on a list of defined actions that when completed confer improvement in outcomes including a shorter length of hospital stay and reduction in complications by up to 50% (11). The pre-operative assessment consultation enables the patient to receive verbal and written information regarding the ERAS ethos with the aim of patient empowerment to understand its rationale. This has been shown to help patients engage with healthcare professionals involved in their care (12).
Prehabilitation
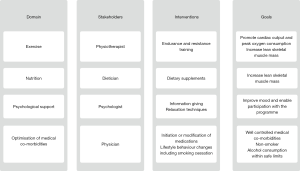
Prehabilitation is a multimodal programme delivered pre-operatively through the four domains of exercise, nutrition, psychological support and optimisation of medical co-morbidities (Figure 1). The response to a surgical stimulus comprises metabolic, immunological and neuroendocrine changes including an increase in oxygen consumption and protein catabolism. The aim of prehabilitation is to promote the patient’s functional capacity by promoting cardiac output and peak oxygen consumption to deal more appropriately with the increased demands of the surgical stress response (13).
Exercise training
Exercise regimens have been devised for patients having elective surgery as part of a prehabilitation programme. There is some evidence that pre-operative exercise can reduce length of hospital stay and postoperative complications in patients having abdominal surgery (14). It has also been shown that exercise interventions can reduce pulmonary morbidity within 30 days of having major abdominal surgery but without any significant difference in length of hospital stay compared to patients who did not enter the prehabilitation programme. It is notable that prehabilitation protocols are varied and there is a current lack of consistency in their approach (15) and in part may explain the mixed evidence base for the effect on patient outcomes.
Pre-operative exercise programmes have been evaluated in cancer patients. A protocol featuring both endurance and resistance training for patients having video-assisted thoracic surgery showed that muscle strength was significantly increased just prior to surgery and at 3 months postoperatively (16). A systematic review has looked at the effect of exercise intervention in cancer patients having neoadjuvant treatment. It found that exercise training in this patient cohort is safe with an adherence rate of 66% to 96% across the range of studies. However, there is insufficient data to enable valid conclusions to be drawn about the ideal format of this intervention and the impact on patient outcomes (17).
Nutrition
It is understood that pre-operative malnutrition is an independent risk factor for postoperative mortality and complications including wound healing (18). Malnutrition is common in the cancer patient with multifactorial aetiology including: reduced appetite due to treatment side effects; malabsorption secondary to gastrointestinal problems including mechanical obstruction and socioeconomic factors including inability to buy varied and healthy foodstuffs. Sarcopenia, defined as a reduction in skeletal muscle mass, is present in 20% to 70% of cancer patients and is associated with patient-reported fatigue, reduced quality of life and mortality. However, it is difficult to identify patients with sarcopenia as 40% to 60% of cancer patients are classified as overweight or obese (19). The presence of muscle fat infiltration, or myosteatosis, has been shown to confer higher mortality and morbidity rates within 30 days of colorectal surgery for cancer (20) and indicates that patients with higher body fat compositions are also at increased risk of postoperative complications.
Hypoalbuminemia measured pre-operatively is a predictor of postoperative mortality and overall complication rate (21). This highlights the importance of screening for malnutrition at the pre-operative assessment including measuring serum albumin and noting the patient’s height and weight in order to calculate their body mass index. This enables prompt referral to a dietician and a strategy delivered to promote protein anabolism (22) including the use of nutritional supplements. One of the fundamental priorities is to increase lean skeletal muscle mass and this can be achieved via the multimodal approach of promoting protein intake and engaging with physical activity.
Psychology and motivation
Cancer patients are at increased risk of living with adverse effects on mental health including depression and anxiety (23). This can have a detrimental impact on engagement with other aspects of prehabilitation. Evaluation of pre-operative psychological interventions, including procedural information and relaxation, appear to show some benefit including reduced postoperative pain and length of hospital stay (24). Another study has found that prehabilitation focusing on psychological interventions correlated with improved mood and reduced fatigue amongst cancer patients (25). However, further evidence is required to confirm these findings. Despite the broad aims of prehabilitation for cancer patients, every individual possesses a unique set of physical, psychological and social needs. Current prehabilitation programmes are heterogenous in terms of how they are structured and delivered (26). It is important that prehabilitation programmes are designed and conducted to be individually relevant and act as a motivator and not as an additional burden to the cancer patient.
Optimisation of medical co-morbidities
The prevalence of patients at increased risk of postoperative pulmonary complications following general anaesthesia in one observational study is 28.4% (27). Examples of postoperative pulmonary complications include pneumonia and acute respiratory distress syndrome, which confer an increase in hospital length of stay and mortality (28). Cancer patients are frequently presenting for surgery with co-morbidities and it is recognised that diseases such as chronic obstructive pulmonary disease and asthma are linked to developing postoperative pulmonary complications. In the context of oncological surgery, there is still the time and opportunity to seek advice from specialists including respiratory physicians if such diseases require optimisation including a change in bronchodilator therapy (28).
Diabetes is a common co-morbidity in patients presenting for oncological surgery and the prevalence of diabetes is rising. It is known that hyperglycemia in the perioperative period is associated with an increase in both mortality and morbidity including postoperative infections. In addition, patients diagnosed with diabetes often have longstanding microvascular and macrovascular diseases that may be exacerbated in the perioperative period including coronary artery disease and chronic kidney disease (29). It is recommended in the UK to postpone elective surgery if the patient has a HbA1c of greater than or equal to 69 mmol/mol (30). This target may not be achievable in the often time critical nature of oncological surgery. However, a multidisciplinary review can still occur between the pre-operative assessment nurse, anaesthetist, general practitioner and diabetologist to initiate or modify prescriptions including insulin and oral hypoglycemic medications in the weeks preceding surgery (29). This highlights the individualistic approach that is required and involves collaboration between the patient and healthcare professionals from both primary and secondary care in order to enable continued monitoring of the changes made.
The predominant cause of mortality and morbidity in the perioperative period relates to a cardiac event such as an acute coronary syndrome (31). Patients presenting for oncological surgery will often have co-morbidities that increase this risk including hypertension, ischaemic heart disease, congestive cardiac failure and arrhythmias. There are published guidelines in the literature that enable the optimisation of the patient’s cardiac function pre-operatively. These include the continuation and cessation, prior to surgery, of medications prescribed for cardiac conditions and the time interval when a cardiac implantable electronic device should be checked pre-operatively (31).
Smoking, through the predominant chemicals of carbon monoxide and nicotine amongst numerous others, is known to increase the risk of postoperative complications including wound infection, pneumonia and an acute coronary syndrome (32). Evidence suggests that patients who stopped smoking at least 3 weeks before their operation had a reduced incidence of wound healing complications but patients who stopped smoking at less than 4 weeks before surgery had a similar risk of postoperative pulmonary complications compared to current smokers (33). However this view has been challenged to suggest there is no clear evidence of harm to stop smoking in the immediate pre-operative period (32). It should be advocated at the pre-operative assessment that smoking cessation is highly recommended and support given accordingly with strategies including behavioral support plus pharmacological intervention including nicotine replacement therapy.
Patients who consume alcohol pre-operatively are at increased risk of complications in the postoperative period including infections, pulmonary complications, increased length of hospital stay and requirement for admission to intensive care (34). A Cochrane Review has found that interventions to reduce or stop alcohol consumption in those patients who consumed an excessive amount of alcohol, defined as more than 21 units per week, did have an impact on abstinence before surgery and a likely reduction in postoperative complications (35). This highlights the importance of screening for current alcohol consumption at the pre-operative assessment visit in order to provide the patient with an opportunity to be advised to reduce their intake if deemed excessive.
The presence of anaemia, defined as a haemoglobin of less than 120 g/L in females and 130 g/L in males, is associated with an increased length of hospital stay and admission to intensive care postoperatively in those patients having non-cardiac surgery (36). Cancer patients are often anaemia and this is particularly prevalent in the colorectal cohort who present with iron deficiency anaemia caused by gastrointestinal bleeding. Due to the often limited time interval from pre-assessment to the date booked for cancer surgery, administration of intravenous iron is gaining prominence in clinical practice to optimise haemoglobin levels and improve outcomes postoperatively. A randomised controlled trial featuring patients having major abdominal surgery has found a 60% reduction in the requirement for an allogeneic blood transfusion in the group given intravenous iron pre-operatively. The study also found that haemoglobin levels were significantly higher by the day of admission for surgery and also at 4 weeks after hospital discharge in the group given intravenous iron pre-operatively (37). This is relevant in the context that allogeneic blood transfusion in the colorectal cancer patient cohort is associated with increased mortality and length of hospital stay (38).
Conclusions
Pre-optimisation of the cancer patient is challenging due to the often time critical nature of organising surgery to promote survival. It has evolved into a multimodal approach with prehabilitation now centre stage to encourage patients to exercise more and adopt a more healthy lifestyle including dietary modifications and smoking cessation. The ethos of healthier living needs to be supported by all members of the multidisciplinary team, including healthcare professionals in both primary and secondary care, in order for this model to be seen as credible by patients and their families.
Prehabilitation is an evolving clinical concept and at present is hindered by a lack of robust trials, particularly in the focused cohort of the cancer patient. There is growing evidence of the benefit of individual elements but how they should be delivered for optimal outcomes is not clear. It could be argued that a standardised approach is also not feasible and that a more tailored approach to each individual cancer patient is potentially needed. There is also the issue of how to best engage with the cancer patient in order to achieve optimal benefit. Current research in this area includes the first randomised controlled trial investigating a multimodal prehabilitation programme with the aim to determine if this interventional approach has an impact on patient functional capacity in addition to postoperative complications (39).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Chris Jones and Leigh Kelliher) for the series “Perioperative Care of the Cancer Patient” published in Digestive Medicine Research. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr-20-48). The series “Perioperative Care of the Cancer Patient” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Office for National Statistics. Cancer registration statistics, England: 2017. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/cancerregistrationstatisticsengland/2017#similar-pattern-in-age-standardised-incidence-rates (Accessed 2nd April 2020).
- Cancer Research UK. Cancer diagnosis and treatment statistics. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/diagnosis-and-treatment#heading-Three (Accessed 2nd April 2020).
- Cancer Research UK. Cancer incidence statistics. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/incidence#heading-Two (Accessed 2nd April 2020).
- Pearse RM, Holt PJE, Grocott MPW. Managing perioperative risk in patients undergoing elective non-cardiac surgery. BMJ 2011;343:d5759. [Crossref] [PubMed]
- Oprea AD, Russell RR, Russell KS, et al. Chemotherapy agents with known cardiovascular side effects and their anesthetic implications. J Cardiothorac Vasc Anesth 2017;31:2206-26. [Crossref] [PubMed]
- Sinclair R, Navidi M, Griffin SM, et al. The impact of neoadjuvant chemotherapy on cardiopulmonary physical fitness in gastro-oesophageal adenocarcinoma. Ann R Coll Surg Engl 2016;98:396-400. [Crossref] [PubMed]
- Davies SJ, Wilson RJT. Preoperative optimization of the high-risk surgical patient. Br J Anaesth 2004;93:121-8. [Crossref] [PubMed]
- Govaert JA, Fiocco M, van Dijk WA, et al. Costs of complications after colorectal cancer surgery in the Netherlands: Building the business case for hospitals. Eur J Surg Oncol 2015;41:1059-67. [Crossref] [PubMed]
- Royal College of Anaesthetists. Preparing for surgery - Fitter Better Sooner. Available online: https://www.rcoa.ac.uk/patient-information/preparing-surgery-fitter-better-sooner (Accessed 2nd April 2020).
- Dhesi JK, Swart M. Specialist pre-operative assessment clinics. Anaesthesia 2016;71:3-8. [Crossref] [PubMed]
- Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg 2017;152:292-98. [Crossref] [PubMed]
- Poland F, Spalding N, Gregory S, et al. Developing patient education to enhance recovery after colorectal surgery through action research: a qualitative study. BMJ Open 2017;7:e013498. [Crossref] [PubMed]
- Banugo P, Amoako D. Prehabilitation. BJA Educ 2017;17:401-5. [Crossref]
- Valkenet K, van de Port IGL, Dronkers JJ, et al. The effects of preoperative exercise therapy on postoperative outcome: a systematic review. Clin Rehabil 2011;25:99-111. [Crossref] [PubMed]
- Kamarajah SK, Bundred J, Weblin J, et al. Critical appraisal on the impact of preoperative rehabilitation and outcomes after major abdominal and cardiothoracic surgery: A systematic review and meta-analysis. Surgery 2020;167:540-49. [Crossref] [PubMed]
- Sebio García R, Yáñez-Brage MI, Giménez Moolhuyzen E, et al. Preoperative exercise training prevents functional decline after lung resection surgery: a randomized, single-blind controlled trial. Clin Rehabil 2017;31:1057-67. [Crossref] [PubMed]
- Loughney L, West MA, Kemp GJ, et al. Exercise intervention in people with cancer undergoing neoadjuvant cancer treatment and surgery: a systematic review. Eur J Surg Oncol 2016;42:28-38. [Crossref] [PubMed]
- Zhong JX, Kang K, Shu XL. Effect of nutritional support on clinical outcomes in perioperative malnourished patients: a meta-analysis. Asia Pac J Clin Nutr 2015;24:367-78. [PubMed]
- Ryan AM, Power DG, Daly L, et al. Cancer-associated malnutrition, cachexia and sarcopenia: the skeleton in the hospital closet 40 years later. Proc Nutr Soc 2016;75:199-211. [Crossref] [PubMed]
- Malietzis G, Currie AC, Athanasiou T, et al. Influence of body composition profile on outcomes following colorectal cancer surgery. Br J Surg 2016;103:572-80. [Crossref] [PubMed]
- Hu WH, Cajas-Monson LC, Eisenstein S, et al. Preoperative malnutrition assessments as predictors of postoperative mortality and morbidity in colorectal cancer: an analysis of ACS-NSQIP. Nutr J 2015;14:91. [Crossref] [PubMed]
- Gillis C, Wischmeyer PE. Pre-operative nutrition and the elective surgical patient: why, how and what? Anaesthesia 2019;74:27-35. [Crossref] [PubMed]
- Niedzwiedz CL, Knifton L, Robb KA, et al. Depression and anxiety among people living with and beyond cancer: a growing clinical and research priority. BMC Cancer 2019;19:943. [Crossref] [PubMed]
- Powell R, Scott NW, Manyande A, et al. Psychological preparation and postoperative outcomes for adults undergoing surgery under general anaesthesia. Cochrane Database Syst Rev 2016;CD008646. [PubMed]
- Treanor C, Kyaw T, Donnelly M. An international review and meta-analysis of prehabilitation compared to usual care for cancer patients. J Cancer Surviv 2018;12:64-73. [Crossref] [PubMed]
- Hijazi Y, Gondal U, Aziz O. A systematic review of prehabilitation programs in abdominal cancer surgery. Int J Surg 2017;39:156-62. [Crossref] [PubMed]
- LAS VEGAS investigators. Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS - an observational study in 29 countries. Eur J Anaesthesiol 2017;34:492-507. [Crossref] [PubMed]
- Lumb AB. Pre-operative respiratory optimisation: an expert review. Anaesthesia 2019;74:43-8. [Crossref] [PubMed]
- Levy N, Dhatariya K. Pre-operative optimisation of the surgical patient with diagnosed and undiagnosed diabetes: a practical review. Anaesthesia 2019;74:58-66. [Crossref] [PubMed]
- Dhatariya K, Levy N, Kilvert A, et al. NHS diabetes guideline for the perioperative management of the adult patient with diabetes. Diabet Med 2012;29:420-33. [Crossref] [PubMed]
- Lee LKK, Tsai PNW, Ip KY, et al. Pre-operative cardiac optimisation: a directed review. Anaesthesia 2019;74:67-79. [Crossref] [PubMed]
- Carrick MA, Robson JM, Thomas C. Smoking and anaesthesia. BJA Educ 2019;19:1-6. [Crossref]
- Wong J, Lam DP, Abrishami A, et al. Short-term preoperative smoking cessation and postoperative complications: a systematic review and meta-analysis. Can J Anaesth 2012;59:268-79. [Crossref] [PubMed]
- Eliasen M, Grønkjær M, Skov-Ettrup LS, et al. Preoperative alcohol consumption and postoperative complications: a systematic review and meta-analysis. Ann Surg 2013;258:930-42. [Crossref] [PubMed]
- Egholm JWM, Pedersen B, Møller AM, et al. Perioperative alcohol cessation intervention for postoperative complications. Cochrane Database Syst Rev 2018;11:CD008343. [PubMed]
- Baron DM, Hochrieser H, Posch M, et al. Preoperative anaemia is associated with poor clinical outcome in non-cardiac surgery patients. Br J Anaesth 2014;113:416-23. [Crossref] [PubMed]
- Froessler B, Palm P, Weber I, et al. The important role for intravenous iron in perioperative patient blood management in major abdominal surgery: a randomized controlled trial. Ann Surg 2016;264:41-6. [Crossref] [PubMed]
- Acheson AG, Brookes MJ, Spahn DR. Effects of allogeneic red blood cell transfusions on clinical outcomes in patients undergoing colorectal cancer surgery: a systematic review and meta-analysis. Ann Surg 2012;256:235-44. [Crossref] [PubMed]
- van Rooijen S, Carli F, Dalton S, et al. Multimodal prehabilitation in colorectal cancer patients to improve functional capacity and reduce postoperative complications: the first international randomized controlled trial for multimodal prehabilitation. BMC Cancer 2019;19:98. [Crossref] [PubMed]
Cite this article as: Robson M, Alexopoulou P. Pre-optimisation of the cancer patient. Dig Med Res 2020;3:29.


