Laparoscopic cholecystectomy for gallbladder polyp is significant in the prevention of gallbladder cancer?
Introduction
Gallbladder polyp is a tumor or tumor-like protrusion of the mucosal surface of the gallbladder. In the general population, the prevalence of the gallbladder polyp is reported to be 4–7% (1-7). The gallbladder polyp is classified as benign and malignant. The benign polyp of the gallbladder consists of the pseudo-tumor (cholesterol and inflammatory polyp, cholesterolosis and adenoma) and the mesenchymatous tumor (fibroma, lipoma and hemangioma). The malignant transformation of the gallbladder polyp is gallbladder cancer. According to the previous study, the majority of the gallbladder polyps are benign and about 90% of the benign polyp is cholesterol poly (8,9).
The most important issue about the clinical significance of the gallbladder polyp is the risk of malignant transformation. This risk is reported to be quite small in these lesions, which are detected mostly incidentally (2,3,7-12). About 5% of the gallbladder polyp is transformed into the gallbladder cancer. The symptoms of the gallbladder cancer are almost unspecific. Because early symptoms of the gallbladder cancer are vague, the gallbladder cancer could be diagnosed frequently at advanced age and the prognosis is very poor. The 5-year survival rate is less than 5% and the overall survival is about 6 months for the advanced stage of gallbladder cancer (12).
The most important issue in deciding the malignant risk of the gallbladder polyp is seemed to be the size of the polyp. The cut-off size is suggested to be 10 mm in most studies and 15 mm according to the other studies. The most of the gallbladder polyp is cholesterol polyp and its size is less than 5 mm (13-15).
The risk of the malignant transformation is increasing to the size of the polyp and the polyp above 1 cm is suspected to be malignant (3,14). According to the previous studies, the malignant incidence was 6% for polyp less than 1 cm, but was increased to be 37.5% for polyp of 1–2 cm. Therefore, the surgery for gallbladder polyp without symptoms may not be necessary and may be observed with ultrasound every 3 months. And the polyps above 10 mm should be resected, irrespective of the clinical symptoms (13).
The gallbladder polyp is the precancerous disease and the surgical indication is suggested to be above 10 mm and the gallbladder polyp above 10 mm should be undergone with the laparoscopic cholecystectomy to prevent the local dissemination of the early cancer of the gallbladder (8,11,15).
The risk factors of the malignant transformation of the gallbladder polyp are the size of above 10 mm, solitary and sessile polyp, coexisting gallstones, the patient age of above 50, and the most important risk factor is rapid growth of the gallbladder polyp (12,16).
The aim of the study was to find out the indication of the laparoscopic cholecystectomy for gallbladder polyp by evaluating the rate of gallbladder cancer detected incidentally, the risk factors of the malignant transformation, and the occurrence rate of the postcholecystectomy syndrome among patients undergoing the laparoscopic cholecystectomy for gallbladder polyp.
Methods
The patients who had taken the laparoscopic cholecystectomy for gallbladder polyp at Pyongyang Medical College Hospital from 2008 to 2018 were enrolled in the study. The demographic and clinical characteristics, and the pathohistological findings and the occurrence rate of the postcholecystectomy syndrome among the patients undertaking the laparoscopic cholecystectomy for gallbladder polyp.
Results
A total of 292 patients who had undergone laparoscopic cholecystectomy for gallbladder polyp were enrolled in the study. The male patients accounted for 40.4% (118 cases) and the female 59.6% (174 cases). The average age of the patients was 39.8±10.2 years (22–69 years). The period between diagnosis and surgery was 4.9±3.6 months (7 days to 12 months).
The case of coexisting gallstone accounted for 4.8% (14 patients).
The reasons of surgery were prevention of gallbladder cancer (65.4%, 191 patients), maldigestion (22.6%, 66 patients), pain (8.2%, 24 patients), fever (2.4%, 7 patients) and nausea (1.4%, 4 patients).
The average operation time was 62.9±18.4 minutes. The postoperative complications were peritoneal bleeding (3.4%, 10 patients), adhesion (1.4%, 4 patients), peritonitis (1%, 3 patients), peritoneal abscess [23.6%, 69 patients including abscess in the gallbladder fossa (62 patients) and right subphrenic abscess (7 patients)], and exudative pleuritis (1.7%, 5 patients). The postoperative hospital stay was 8.1±3.1 days.
The occurrence rate of the postcholecystectomy syndrome was 18.8% (55 out of 292 patients) and the main complaints were maldigestion (17.8%, 52 patients) and pain in the right upper quadrant (13%, 38 patients). The postcholecystectomy syndrome mostly occurred in 6 months after surgery (78.2%, 43 out of 55 patients).
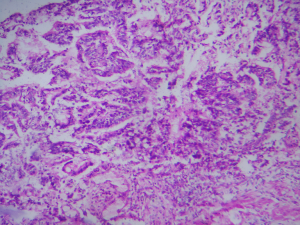
The incidence of gallbladder cancer detected incidentally for resected gallbladder polyps was 6.8% (20 patients). The gallbladder cancer confirmed incidentally was all papillary adenocarcinoma (20 cases), of which the high-differentiated type was 50% (10 cases).
The incidence of gallbladder polyp as benign tumors confirmed pathohistologically was inflammatory polyp 29.4% (80 cases), papillary adenoma 56.2% (153 cases), papillary-tubular adenoma 1.5% (4 cases), adenomatous polyp 10.3% (28 cases) and glandular polyp 2.6% (7 cases).
The rate of malignant transformation to the age was the age of thirties 9.8% (9 out of 92 patients), fifties 22.6% (7 out of 31 patients) and sixties 44.4% (4 out of 9 patients).
There were no cases of coexisting gallstone among patients with gallbladder cancer confirmed incidentally.
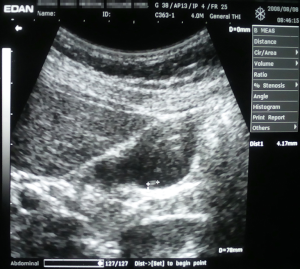
As shown in Table 1, the rate of malignant transformation to the size of the polyp was less than 10 mm 1.4% (3 out of 219 patients), 10–20 mm 12.5% (8 out of 64 patients) and above 20 mm 100% (9 out of 9 patients). Two cases of gallbladder cancer for less than 10 mm were less than 5 mm (4, 5 mm) (Figures 1,2).
Table 1
| Risk | Size, n (%) | Total, n (%) | ||
|---|---|---|---|---|
| Less than 10 mm | 10−20 mm | Above 20 mm | ||
| Benign | 216 (98.6) | 56 (87.5) | − | 272 (93.2) |
| Malignant | 3 (1.4) | 8 (12.5) | 9 (100.0) | 20 (6.8) |
| Total | 219 (100.0) | 64 (100.0) | 9 (100.0) | 292 (100.0) |
The rate of malignant transformation to the number of the polyp was solitary polyp 7.2% (7 out of 97 patients) and multiple polyps 6.7% (13 out of 195 patients).
Discussion
Gallbladder polyp is a protrusion of the gallbladder mucosa into the interior of the gallbladder and its significance is the risk of malignancy. The gallbladder cancer is a lethal disease and it has no special symptoms. Most of gallbladder cancer is diagnosed in the advanced stage and its survival rate is low. Five-year survival rate is 5% and the overall survival is only 6 months (12). The simple cholecystectomy is enough for T1 gallbladder cancer. The incidental gallbladder cancer is detected accidentally in the resected gallbladder polyps among patients undergoing the laparoscopic cholecystectomy for gallbladder polyps. It is the early stage of gallbladder cancer and is enough for the laparoscopic cholecystectomy, and its 5-year survival rate is nearly 100%. So it is very important to decide the surgical indication of the laparoscopic cholecystectomy among patients diagnosed with gallbladder polyps.
According to the literature, the gallbladder polyp is a pre-malignant disease and it is detected among 5% of gallbladder polyp patients (12). In this study, the gallbladder cancer was diagnosed among 20 out of 292 patients (6.8%) undergoing the laparoscopic cholecystectomy for gallbladder polyps. There was no significant difference from the previous literature.
It is generally believed that a gallbladder polyp itself is asymptomatic and the clinical manifestation is due to the accompanying cholelithiasis and cholecystitis. Two possible mechanisms may explain dyspeptic symptoms or attacks of biliary colic. Firstly, the symptoms may be caused by a prolapse of the adenoma into Hartmann’s pouch and then spontaneously reducing itself and secondly, the clinical presentation may be related to the breaking off of a portion of adenoma, which lying free into the lumen of the gallbladder could obstruct the cystic duct (8,13). The symptoms in the gallbladder polyps are no symptoms 11.3% (33 patients), right upper quadrant pain 58.9% (172 patients), nausea 40.8% (119 patients), epigastric discomfort 32.2% (94 patients) and others 18.5% (54 patients) (17). According to another report, there are right upper quadrant or epigastric pain (98%), nausea and vomiting (51%), dyspepsia (26%) in the gallbladder polyps and the most of physical symptoms is right upper quadrant pain (61%) (11). In this study, the reasons to take operations for gallbladder polyps are the case taking surgical advice for prevention of gallbladder cancer 65.4% (191 out of 292 patients), dyspepsia 22.6% (66 patients), biliary colic 8.2% (24 patients), fever 2.4% (7 patients) and nausea 1.4% (4 patients). The case of no symptoms is overwhelming and the dyspepsia (22.6%) is the most of the symptoms in the patients undergoing cholecystectomy for gallbladder polyps compared with the previous reports.
The important factors in evaluating the malignant risk of gallbladder polyps are size of polyp above 10 cm, solitary and sessile polyp, accompanied gallstones, patient’s age of above 50 years and the patients with gallbladder polyp above 10 cm should take laparoscopic cholecystectomy (12,16,18-22).
The most important factor in deciding the malignant risk of gallbladder polyps is the size of the polyp. The cut-off size is suggested to be 10 mm in most studies and 15 mm according to some other studies and the patients with gallbladder polyps of above 10 mm should take laparoscopic cholecystectomy (8,15,23). In this case, the size of polyps is less than 10 mm 1.4% (3 out of 219 patients), 10 to 20 mm 12.5% (8 out of 64 patients) and above 20 mm 100% (9 out of 9 patients) in 20 patients diagnosed with gallbladder cancer. It was accordant with the previous literatures. In total, 20.6% of the benign polyp (56 out of 272 patients) and 85% of the malignant polyp (17 out of 20 patients) was above 10 mm.
Most of gallbladder polyps is the cholesterol polyp that is less than 5 mm in the size. According to the studies, it should be considered to perform follow-up US every 3 months in the gallbladder polyps measuring less than 10 mm and the asymptomatic gallbladder polyps measuring less than 6 mm have no risk of malignancy and the follow up is unnecessary (13,24). In this study, 3 cases of gallbladder polyp were less than 10 mm are diagnosed with gallbladder cancer and 2 cases were less than 5 mm. That is why, though less than 5 mm, there is risk of malignancy and necessity for laparoscopic cholecystectomy on the gallbladder polyps less than 5 mm.
Some studies found out that gallbladder polyps are more in male than in female and one of the malignant risk factors for gallbladder polyps is male (8,23). Our study included 118 males (40.4%) and 174 females (59.6%), and the gallbladder polyps are in female more than in male. The gallbladder carcinoma is diagnosed in 10 out of 118 males and in 10 out of 174 females, and there was no difference between in male and female in the malignant risk to the sex.
The gallbladder cancer is diagnosed in 9 out of 92 patients (9.8%) aged thirties, in 7 out of 31 patients (22.6%) aged fifties, and in 4 out of 9 patients (44.4%) aged sixties.
Most studies suggested that one of the malignant risk factors for gallbladder polyps is accompanied gallstone (8,16,25). In this study, there was no case accompanied with gallstone in the gallbladder polyp patients confirmed with gallbladder cancer.
The previous literatures confirmed that a solitary polyp is one of the malignant risk factors (1,7,9,10,18,21,22). In this study, the solitary and multiple polyp was 7.2%, 6.7% and there were no differences between in solitary and multiple polyps.
Our study found out that malignant risk factors of gallbladder polyps are the size of the polyp and the age of patients. However, though the size is less than 5 mm, the malignant risk cannot be excluded and it is reasonable to take laparoscopic cholecystectomy for gallbladder polyps.
Postcholecystectomy syndrome is defined as the recurrence of symptoms similar to those experienced before the cholecystectomy. The incidence of postcholecystectomy syndrome has been reported to be as high as 40% (2–47%) in one study. Postcholecystectomy syndrome occurs in the early period or in the late period after operation, or sometimes after several months or years. This usually takes the form of right upper quadrant abdominal pain and dyspepsia and in details, abdominal pain of biliary and non-biliary cause, gastrointestinal symptoms including dyspepsia and vomiting, jaundice and fever. More severe symptoms occur due to postcholecystectomy complications (26-30).
In this study, the incidence of postcholecystectomy was 18.8% (55 out of 292 patients) and the symptoms were dyspepsia (17.8%, 52 patients), slight pain in the right upper quadrant (13.0%, 38 patients). The incidence was not so high and there was no symptoms such as fever, jaundice, diarrhea, nausea, vomiting and weight loss. There was no loss of working ability due to postcholecystectomy syndrome. The onset period of postcholecystectomy syndrome was 6 months (78.2%, 43 out of 55 patients) and over 6 months (21.8%, 12 out of 55 patients). There was no postcholecystectomy syndromes in the perioperative period.
Conclusions
The gallbladder polyp is pre-malignant disease and the malignant risk factors are the size of polyp and the age of patients. However, though the size is small, the risk of malignancy cannot be excluded and the incidence of postcholecystectomy syndrome is not so high and the postcholecystectomy doesn’t influence on the quality of life, that is why, once the gallbladder polyps are diagnosed, it would be suggested to take laparoscopic cholecystectomy actively.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2019.10.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All procedures performed in our studies involving patients were in accordance with the ethical standards of the national medical committee of DPRK (No. 02-1221). We obtained informed consents from all patients in accordance with national medical rules of DPRK.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chattopadhyay D, Lochan R, Balupuri S, et al. Outcome of gallbladder polypoidal lesions detected by transabdominal ultrasound scanning: a nine year experience. World J Gastroenterol 2005;11:2171-3. [Crossref] [PubMed]
- Csendes A, Burgos AM, Csendes P, et al. Late follow-up of polypoid lesions of the gallbladder smaller than 10 mm. Ann Surg 2001;234:657-60. [Crossref] [PubMed]
- Bayram Kabaçam G, Akbıyık F, Livanelioğlu Z, et al. Decision for surgery in the management of a rare condition, childhood gallbladder polyps, and the role of ultrasonography. Turk J Gastroenterol 2013;24:556-60. [Crossref] [PubMed]
- Inui K, Yoshino J, Miyoshi H. Diagnosis of gallbladder tumors. Intern Med 2011;50:1133-6. [Crossref] [PubMed]
- Jørgensen T, Jensen KH. Polyps in the gallbladder. A prevalence study. Scand J Gastroenterol 1990;25:281-6. [Crossref] [PubMed]
- Kratzer W, Haenle MM, Voegtle A, et al. Ultrasonographically detected gallbladder polyps: a reason for concern? A seven-year follow-up study. BMC Gastroenterol 2008;8:41. [Crossref] [PubMed]
- Myers RP, Shaffer EA, Beck PL. Gallbladder polyps: epidemiology, natural history and management. Can J Gastroenterol 2002;16:187-94. [Crossref] [PubMed]
- Matos AS, Baptista HN, Pinheiro C, et al. Gallbladder polyps: How should they be treated and when? Rev Assoc Med Bras 2010;56:318-21. [Crossref] [PubMed]
- Sun XJ, Shi JS, Wang JS, et al. Diagnosis and treatment of polypoid lesions of the gallbladder: report of 194 cases. Hepatobiliary Pancreat Dis Int 2004;3:591-4. [PubMed]
- Josef E, Fischer MD. Mastery of surgery. 5th ed. Philadelphia: Lippincott Willimas & Wilkins; 2006:1025.
- Ljubičić N, Zovak M, Doko M, et al. Management of gallbladder polyps: an optimal strategy proposed. Acta Clin Croat 2001;40:57-60.
- Dixit VK, Babu AV. Carcinoma of Gallbladder. J Gastrointest Dig Sys 2015;5:310.
- Farinon AM, Pacella A, Cetta F, et al. "Adenomatous polyps of the gallbladder" adenomas of the gallbladder. HPB Surg 1991;3:251-8. [Crossref] [PubMed]
- Koga A, Watanabe K, Fukuyama T, et al. Diagnosis and operative indications for polypoid lesions of the gallbladder. Arch Surg 1988;123:26-9. [Crossref] [PubMed]
- Carrillo N, Central MP. Gallbladder Polyps, Surgical Indications According to their Size and Morphology. Gastroenterol Hepatol Open Access 2015;2:00035.
- Randi G, Franceschi S, La Vecchia C. Gallbladder cancer worldwide: geographical distribution and risk factors. Int J Cancer 2006;118:1591-602. [Crossref] [PubMed]
- Akyürek N, Salman B, Irkorucu O, et al. Ultrasonography in the diagnosis of true gallbladder polyps: the contradiction in the literature. HPB 2005;7:155-8. [Crossref] [PubMed]
- Chijiiwa K, Tanaka M. Carcinoma of the gallbladder: an appraisal of surgical resection. Surgery 1994;115:751-6. [PubMed]
- Mangel AW. Management of gallbladder polyps. South Med J 1997;90:481-3. [Crossref] [PubMed]
- Reck T, Kockerling F, Heyder N, et al. Polypoid lesions of the gallbladder: preventive cholecystectomy? Chirurg 1992;63:506-10. [PubMed]
- Shinkai H, Kimura W, Muto T. Surgical indications for small polypoid lesions of the gallbladder. Am J Surg 1998;175:114-7. [Crossref] [PubMed]
- Yang HL, Sun YG, Wang Z. Polypoid lesions of the gallbladder: diagnosis and indications for surgery. Br J Surg 1992;79:227-9. [Crossref] [PubMed]
- Cha BH, Hwang JH, et al. Pre-operative factors that can predict neoplastic polypoid lesions of the gallbladder. World J Gastroenterol 2011;17:2216-22. [Crossref] [PubMed]
- Pedersen MR, Dam C, Rafaelsen SR. Ultrasound follow-up for gallbladder polyps less than 6 mm may not be necessary. Dan Med J 2012;59:A4503. [PubMed]
- Beck PL, Shaffer EA, Gall DG, et al. The natural history and significance of ultrasonographically defined polypoid lesions of the gallbladder in children. J Pediatr Surg 2007;42:1907-12. [Crossref] [PubMed]
- Mergener K, Clavien PA, Branch MS, et al. A stone in a grossly dilated cystic duct stump: a rare cause of postcholecystectomy pain. Am J Gastroenterol 1999;94:229-31. [Crossref] [PubMed]
- Girometti R, Brondani G, Cereser L, et al. Postcholecystectomy syndrome: spectrum of biliary findings at magnetic resonance cholangiopancreatography. Br J Radiol 2010;83:351-61. [Crossref] [PubMed]
- Terhaar OA, Abbas S, Thomton FJ, et al. Imaging patients with ‘‘post-cholecystectomy syndrome’’: an algorithmic approach. Clin Radiol 2005;60:78-84. [Crossref] [PubMed]
- Lum YW, House MG, Hayanga AJ, et al. Postcholecystectomy syndrome in the laparoscopic era. J Laparoendosc Adv Surg Tech A 2006;16:482-5. [Crossref] [PubMed]
- Zhou PH, Liu FL, Yao LQ, et al. Endoscopic diagnosis and treatment of postcholecystectomy syndrome. Hepatobiliary Pancreat Dis Int 2003;2:117-20. [PubMed]
Cite this article as: Ryong H, Jang GC, Ryu DM, Ji CS. Laparoscopic cholecystectomy for gallbladder polyp is significant in the prevention of gallbladder cancer? Dig Med Res 2019;2:32.