Pre-assessment and pre-optimisation of the surgical patient
Introduction
Pre-assessment clinics are usually the first contact the patient has with the anaesthetic team in their surgical journey. In many centres the clinic is nurse-led with supportive anaesthetic clinical input from clinicians with particular interest. Many also offer face-to-face high-risk, consent or multi-disciplinary anaesthetic clinics. Pre-assessment, therefore, is a prime opportunity for patients to undergo a detailed assessment, and might highlight patients whom are medically more complex and have multiple co-morbidities. These patients may require further focused input from other medical specialist services to manage their chronic illnesses and/or optimise other conditions peri-operatively. Increasingly useful is the opportunity to engage patients in smoking cessation programmes and reducing their alcohol intake pre-operatively, helping improve outcomes.
The pre-operative clinic also allows comprehensive assessment of those conditions in the context of the proposed surgery to help calculate of risk. Various toolkits are available and may prove useful to help create a conversation surrounding consent and facilitate the process of shared decision-making (1). Furthermore it is also an opportune moment to educate patients about the concept of ERAS, thus prepare them for surgery and help manage their expectations, as patient engagement is paramount for it to be successful.
Anaemia
Reported incidence of anaemia have suggested that up to a third of patients that present to pre-operative assessment are anemic. There is a large body of evidence that demonstrates that pre-operative anaemia is associated with an increased risk of 30-day morbidity and mortality. A retrospective cohort study carried out by Musallam et al. which included >220,000 patients demonstrated that even mild anaemia, when compared to moderate and severe anaemia, was linked to worse peri-operative outcomes (2,3). The European Surgical Outcomes study (EuSOS) showed similar outcomes for patients with anaemia undergoing major surgery. Their dataset of >46,000 patients demonstrated prolonged hospital stays and higher rates of intensive care admissions (4). Metanalysis have also shown that just a 10 g/L drop in haemoglobin is associated with a 43% increased risk of red cell transfusion, and the associated complications and increased mortality linked with it (5).
ERAS has long identified anaemia as a goal for pre-optimisation. Moreover efforts to reduce the need for peri-operative blood transfusion is key. Not only are blood transfusions associated with a number of complications, leading to an increase in length of stay, it is also an expensive and finite source (2).
In recent years the World Health Organisation (WHO) now advocates that the principles of Patient Blood Management (PBM) should be used to optimise a patient’s own blood volume (5), this also includes optimising pre-operative anaemia in the prior to planned surgery. PBM is a logical multi-disciplinary team concept and focuses on 3 pillars of care—the first of which concentrates on the pre-operative detection, investigation and management of anaemia (6).
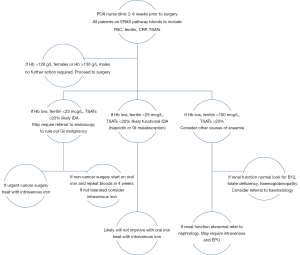
Routine full blood count (FBC) should be taken as early as possible, ideally at least 4–6 weeks before major surgery, therefore affording time to treat. It may be useful at this stage to include haematinics, serum ferritin and C-reactive protein. Those patients found to be anemic may require further investigations to assess the cause of anaemia.
The causes of anaemia can be acute or chronic, and are sometimes multi-factorial. Simple blood tests [FBC, serum ferritin and Transferrin Saturations (TSATs)] can help elucidate the type of anaemia and guide management. Iron deficiency anaemia (IDA) is most common worldwide, commonly found in the surgical population and usually identified as a microcytic form (MCV <80fl). Iron stores are low, often due to ongoing losses, or poor dietary intake. Functional iron deficiency is recognized as a condition where red blood cells cannot utilise the body’s iron stores creating an anemic profile. Iron mobilization is governed by hepcidin production in the liver. Inflammatory conditions including cancers can upregulate hepcidin production, which decreases available iron by interrupting absorption from gut and existing stores thus reducing its availability to red blood cells. Other forms of microcytic anaemia include renal disease where there is reduced haemopoeisis and haemoglobinopathies. Macrocytic anaemia (MCV >96fl) is typically linked to folate and B12 deficiencies, as well as excess alcohol. Anaemia related to chronic diseases is usually normocytic in nature (MCV 80-96fl) (6).
A large proportion of surgical patients have iron deficiency anaemia, or functional IDA, often secondary to their presenting surgical problem. This can be easily managed in the pre-operative period, but may need to be expedited. Oral iron therapy is a simple, cost effective way to treat absolute iron deficiency anaemia, however it is poorly tolerated by patients leading to poor compliance. More importantly it also requires up to 3 or more months treatment to achieve sufficient iron stores (6), which may not be achievable in some urgent cancer surgery. An alternative to both forms of IDA is parenteral iron therapy, which has increasingly been shown to be a safe and effective method in the treatment, with fewer side effects and often better tolerated. Serious adverse events are rare; 38 per 1,000,000 which is favourable when compared to 1 in 100,000 risk of death related to transfusions calculated by the Serious Hazards of Transfusion (SHOT) reports in the U.K. As a result the European Medicines Agency agree that the benefits outweigh the risks when used appropriately (7). The cost implications have not been widely investigated, however Bhandari et al. compared administration of intravenous iron with RBC transfusion and found that intravenous iron led to a net saving (7).
More recently the Peri-Operative Quality Improvement Programme (PQIP), affiliated to the RCOA, maintains that a key priority should be the identification and management of peri-operative anaemia. It has endorsed that hospitals should create a standardized peri-operative anaemia pathway to allow maximum optimisation of anaemia. Newer recommendations have also been made to target the same haemoglobin value in men and women. Both are equally likely to bleed, and women have a comparably smaller blood volume and so consequently will become more anemic for any given blood loss. There is also evidence that women with pre-operative anaemia can have worse outcomes (2).
The concept of an anaemia pathway is still relatively new and in the process of setting it up there may be several barriers. It requires a multi-disciplinary approach that needs to start within primary care, and thus early liaison is very important. Early referral can lead to early intervention and maximise the timeframe over which anaemia can be optimised. Within secondary care various teams need to be engaged for the pathway to work efficiently. This includes haematologists who are key in helping develop an anaemia pathway. There also needs to be communication with the teams (e.g., gastroenterology teams managing patients with inflammatory bowel disease) that run existing iron infusion services who may be able to help co-ordinate and accommodate the pre-operative patient population (2).
Often pre-assessment anaesthetists and nurses have been the pivotal players in helping co-ordinate this pre-operative anaemia service, but it is recognized that needs may vary between hospitals. Many units within the U.K. have already set up anaemia pathways in accordance with national guidance. At our centre the identification and management of pre-operative anaemia is coordinated through pre-assessment clinicians. Where possible screening is done at earlier points on the patient journey e.g., endoscopy. The pathway incorporates close liaison with specialist nurses from surgical teams, further investigations as required. Treatment takes place using day unit facilities for a short appointment, when necessary, with parenteral iron infusions. Such pathways, for example Figure 1, provide an invaluable addition to part of the enhanced recovery programme to reduce length of stay, as well as reduce overall morbidity and mortality related to pre-operative anaemia.
Diabetes
Diabetes is increasing in prevalence with approximately 3.8 million people in the U.K. living with this chronic condition and nearly a further million with undiagnosed diabetes. These patients have an increase in length of stay and are more likely to have post-operative complications. Pre-operative management and optimisation of diabetes can lead to a decrease in complications and mortality. Consequently it has been recommended that HbA1c concentrations should be optimised prior to elective surgery, if possible (8).
NICE guidelines suggest that all patients have a HbA1c recorded within 3 months of surgery. However data from the PQIP annual report 2017–2018 reveal only 69% of patients have a pre-operative HbA1c, this is a key element that needs improvement to allow maximal optimisation (7). Review of glycemic control and subsequent optimisation should therefore start at the point of referral for surgical consultation. This then allows time for any improvement, which may take months. Treatment will involve the multidisciplinary team and support services and should continue throughout the patient journey from primary care through to secondary care and then onto discharge. The pre-operative assessment can provide a useful platform to ensure that optimisation is facilitated and ongoing prior to surgery and organise post-operative care plans alongside.
Peri-operative hypoglycaemia and hyperglycaemia are linked to harm and death and every effort should be made to avoid both. Therefore careful consideration should be made pre-operatively of how to manage a patient’s diabetes in the peri-operative period and this can be done in conjunction with the diabetes team and documented so that any issues with glycemic control can be managed as necessary from the point of admission (8).
Diabetes should also not be considered in isolation as it is often associated with other co-morbidities including cardiovascular disease, peripheral vascular disease, renal disease, hypertension and obesity (8). These are also associated with increase in surgical complications and morbidity and optimisation of these in the pre-operative period can also lead to improvements in outcomes (8). There are multiple national guidelines with recommendations of optimal management of these conditions in isolation, however there needs to careful consideration of all of these in context of the surgical journey to diminish the potential for any peri-operative adverse events as a consequence of drug-disease or drug-drug interactions (7) and the pre-operative assessment can present an opportune moment to evaluate these.
Smoking cessation and abstinence from alcohol
It is well known that smoking is detrimental to an individual’s health and is the single biggest cause of premature and preventable death in the U.K (9). Smoking is associated with worse surgical outcomes, and inevitably patients are at an increased risk of cardio-respiratory complications and post-operative complications including infections and poor wound healing. As a consequence they have longer hospital admissions and are more likely to require intensive care admission (9).
Evidence suggests that the optimum time to quit smoking is 2 months prior to surgery. For those that can not, or are not willing to, stop smoking are advised to stop for at least 2 weeks prior to surgery, and not to smoke on the day of surgery (9). Pre-assessment can refer patients to specialist smoking cessation services, as well as educate and counsel patients with regards to this, and encourage stopping smoking as part of the ERAS pathway.
Excessive alcohol consumption is also associated with worse surgical outcomes with a staggering 56% increase in post-operative morbidity (comparing high alcohol consumption, which is defined as >36 grams of alcohol per day, to those who are abstinent or have lower alcohol consumption). The adverse effects can include abnormalities of the biochemistry, alteration of drug kinetics and acute withdrawal, all of which can lead to post-operative complications and increased length of stay (10). There is evidence that >1 month abstinence reduces these (11).
Chronic alcohol use can be associated with multiple co-morbidities including cardiovascular disease (in particular hypertension, arrhythmia and alcohol related cardiomyopathies) and pathology of the nervous system including autonomic or peripheral neuropathies (12).
It would be prudent to try and identify these at risk patients as early as possible, and where practicable to try to highlight these before attending surgical pre-assessment through patient questionnaires in the community. However through simple screening the pre-operative nurse assessment does allow identification of those patients with high alcohol consumption. Support and advice face-to-face and through liaison services can help to help reduce consumption and promote the benefits of abstinence. ERAS guidelines would encourage stopping drinking for >1 month pre-operatively to improve outcomes (11).
Further detailed examination of any associated co-morbidities can be investigated and optimised appropriately. At our centre this risk assessment questionnaire takes place at every consultation in pre-assessment and helps establish which patients are more likely to have an acute withdrawal, ensuring alcohol liaison services are alerted and planned, and even prescriptions written to manage the symptoms pre-emptively.
Prehabilitation
It appears intuitive that enhancing a patient’s cardio-respiratory function would have a positive benefit on post-operative outcomes. Improving physical capacity is advantageous in almost all health and medical conditions and there is strong evidence to support this (13). Re-analysis of a pilot study, from 2010–2015, examined patients undergoing tri-modal prehabilitation (including exercise, nutrition and psychological support) and demonstrated a significant improvement in functional capacity when compared to those undergoing rehabilitation only (a tri-modal programme post-operatively) (13). Evidence is also emerging that prehabilitation can decrease post-operative complications which is the fourth principle behind ERAS. Not only can it prepare patients for surgery but can be beneficial in preparing them for other treatment that they be undergoing for management of their cancer, in particular chemotherapy or radiotherapy as both these can commonly cause de-conditioning (14).
Prehabilitation is described as “ a process on the cancer continuum of care that occurs between the time of cancer diagnosis and the beginning of acute treatment and includes physical and psychological assessments that establish a baseline functional level, identify impairments and provide interventions that promote physical and psychological health to reduce the incidence and/or severity of future impairments” (14).
The aim of pre-operative conditioning is to improve function and physiological capacity enough to allow patients to withstand the stress of a surgical insult and facilitate the post-operative recovery (15). Multimodal prehabilitation has been shown to improve functional capacity compared with unimodal models and considers the complex interactions between physical and psychological health of a patient. These multimodal models also include nutrition as an important aspect and can prepare patients physically and emotionally for major surgery (14).
Metanalysis by Hughes at al looked at 15 randomised control trials with 457 patients undergoing a prehabilitation programme. Two of these trials incorporated the programme as part of their peri-operative ERAS pathway (16). There was a notable reduction in the overall morbidity, which was statistically significant (P=0.005) as well as a reduction in the pulmonary complications in the prehabilitation group (16). Their conclusion from this was that prehabilitation would be beneficial if routinely implemented, however further work is required to establish optimal rehabilitation protocols.
In the U.K. there are several units that have set up prehabilitation programmes. The south coast region are currently recruiting patients to their ‘Wessex fit 4 cancer surgery trial” (17). The patient compliance is up to 96%, and feedback has been very positive thus far, recruiting more than 100 patients to date. While the “PREPARE programme” run by Imperial College Healthcare NHS Trust incorporates prehabilitation with their ERAS programme. It follows the trimodal model of prehabilitation and includes a tailored exercise programme, nutritional support and advice from a dietician and finally psychological support with regular contact with a clinical nurse specialist and giving patients and carers ample opportunities to discuss any anxieties related to their treatment. Between 2015 and 2018 approximately 100 patients have enrolled into the programme with more than a 50% reduction in pulmonary complications (from 60% in 2015 to 18% in 2018) and in the same time frame a fall in median length of stay from 14 to 8 days (18). These programmes are testament to the benefits of prehabilitation and further work needs to be done over the next few years to assess how to structure these programmes so that they can form part of the standard of care provided for patients undergoing major cancer surgery.
Lastly, concept of shared decision making
It would be remiss, in the current climate, to not discuss the concept of shared decision-making in the context of pre-operative assessment. As mentioned at the start, patient involvement and engagement is essential in the process of enhanced recovery. Shared decision-making is a dialogue and process that runs through the patients treatment journey. It brings together the patient’s own beliefs and thoughts about their healthcare with the expertise of those treating them to formulate an individual package of care (19).
As a concept it has been in the literature since the 1980’s, but it is only in the last 5–10 years that it is a practice that is being embraced and incorporated as part of the standard of care. Anaesthetists are ahead of the curve where consent is concerned, however are still lagging behind in terms of the patient-centred care aspect of shared decision-making (19). The main issue being time. Unfortunately this is often lacking especially when meeting patients for the 1st time on the day of surgery. This is where pre-assessment can provide an opportunity to explore a patient’s thoughts and beliefs with regards to their own health and allows the clinician to assess the patient. This is particularly useful with the high-risk surgical patient with multiple co-morbidities. It gives time to risk assess and have frank conversations with the patient. It is also a time to prepare patients for what to expect, especially in terms of an enhanced recovery programme. It is an empowering process for them as they feel they that they have some control but it is also an important time to ensure that their expectations are managed. The main challenge, in a service -driven era, will be finding the time to fully implement and embrace shared decision making as part of a standard of care.
Final thoughts
As explored and discussed throughout, pre-assessment and pre-optimisation of the patient is a key element in the enhanced recovery process. It ensures that the patient is at their optimum to withstand major surgery and with an ultimate aim to reduce morbidity and mortality in these high risk patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Chris Jones, Chuangqi Chen and Xuefu Zhou) for the series “Enhanced Recovery After Surgery (ERAS) Program in General Surgery” published in Digestive Medicine Research. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2019.09.02). The series “Enhanced Recovery After Surgery (ERAS) Program in General Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Guidelines for the Provision of Anaesthesia Services for Preoperative Assessment and Preparation 2019 (website accessed 06.06.19). Available online: https://www.rcoa.ac.uk/system/files/GPAS-2019-02-PREOP.pdf
- Addressing preoperative anaemia: Ten top tips, practical advice and the evidence base” (website accessed 15.07.19). Available online: https://pqip.org.uk/pages/0
- Musallam KM, Tamim HM, Richards T, et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet 2011;378:1396-407. [Crossref] [PubMed]
- Baron DM, Hochrieser H, Posch M, et al. Preoperative anaemia is associated with poor clinical outcome in non-cardiac surgery patients. Br J Anaesth 2014;113:416-23. [Crossref] [PubMed]
- Munting KE, Klein AA. Optimisation of pre-operative anaemia in patients before elective major surgery - why, who, when and how?. Anaesthesia 2019;74:49-57. [Crossref] [PubMed]
- Thakra SV., Clevenger B, Mallett S. Patient Blood Management and Peri-operative Anaemia. BJA Educ 2017;17:28-34. [Crossref]
- Muñoz M, Acheson AG, Auerbach M, et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia. 2017;72:233-47. [Crossref] [PubMed]
- Levy N, Dhatariya K. Pre-operative optimisation of the surgical patient with diagnosed and undiagnosed diabetes: a practical review. Anaesthesia 2019;74:58-66. [Crossref] [PubMed]
- Joint Briefing: Smoking and surgery (website accessed 05.07.19). Available online: https://www.rcoa.ac.uk/sites/default/files/Joint-briefing-Smoking-Surgery.pdf
- Budworth L, Prestwich A, Lawton R, et al. Preoperative Interventions for Alcohol and Other Recreational Substance Use: A Systematic Review and Meta-Analysis. Front Psychol 2019;10:34. [Crossref] [PubMed]
- Jankowski CJ. Preparing the Patient for Enhanced Recovery After Surgery. Int Anesthesiol Clin 2017;55:12-20. [Crossref] [PubMed]
- Chapman R, Platt F. Alcohol and Anaesthesia. BJA Educ 2009;9:10-3.
- Minnella EM, Bousquet-Dion G, Awasthi R, et al. Multimodal prehabilitation improves functional capacity before and after colorectal surgery for cancer: a five-year research experience. Acta Oncol 2017;56:295-300. [Crossref] [PubMed]
- Scheede-Bergdahl C, Minnella EM, Carli F. Multi-modal prehabilitation: addressing the why, when, what, how, who and where next?. Anaesthesia 2019;74:20-6. [Crossref] [PubMed]
- Gillis C, Li C, Lee L, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 2014;121:937-47. [Crossref] [PubMed]
- Hughes MJ, Hackney RJ, Lamb PJ, et al. Prehabilitation Before Major Abdominal Surgery: A Systematic Review and Meta-analysis. World J Surg 2019;43:1661-8. [Crossref] [PubMed]
- Wessex Fit-4 Cancer Surgery (Website accessed 07.06.19). Available online: http://www.wesfit.org.uk/
- PREPARE programme (website accesses 07.06.19). Available online: https://www.imperial.nhs.uk/our-services/cancer-services/oesophago-gastric-cancer/prepare-programme
- Sturgess J, Clapp JT, Fleisher LA. Shared decision-making in peri-operative medicine: a narrative review. Anaesthesia 2019;74:13-9. [Crossref] [PubMed]
Cite this article as: Das M, Blightman K. Pre-assessment and pre-optimisation of the surgical patient. Dig Med Res 2019;2:30.