
Epithelioid hemangioendothelioma of the liver—case report
Introduction
Epithelioid hemangioendothelioma of the liver (EHL) is a rare vascular tumor of epithelioid origin (1). The tumor occurs among people from 19–86 years of age, and is twice as more frequent in male than in female patients (2). The tumor has variable biology, ranged from benign haemangioma to highly malignant angiosarcoma, thus it is very difficult to prognose the outcome. The etiology is not clear yet, and the risk factors such as hormone contraceptives, liver trauma, vinyl-chloride and others are considered (1,3). The range of the tumor features varies from completely asymptomatic to liver insufficiency (4). The diagnosis is rarely confirmed by the initial diagnostic work-up, and the misdiagnosis of a metastasis or other more common liver tumors are primarily taken into account. Definitive diagnosis proven by pathohistology is therefore an unexpected outcome in most cases (1,3).
Case presentation
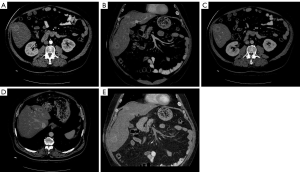
A 59-year-old Caucasian male patient was admitted to University Hospital Merkur for diagnostic work-up and liver transplantation (LT). The first symptoms occurred in 2014 and the patient was presented with sudden loss of consciousness, fatigue and right upper abdominal pain. By the end of 2016, liver magnetic resonance (MR) and multislice computed tomography (MSCT) revealed multiple focal lesions up to 2 cm in diameter in the 3rd, 4th, 5th and 7th liver segment (Figure 1).
Four biopsies were performed during the diagnostic process. Three of them were negative considering EHL final diagnosis and they confirmed active hepatitis and cirrhosis. Immediately after discovering suspicious lesions on MSCT, a third biopsy was performed and it revealed immunohistochemically tumor positive cells for CD31, CD34, F-VIII and D2-40. It finally confirmed hematoxylin and eosin staining (HE) (Table 1).
Table 1
| Biopsy number | Biopsy method (staining) | Findings/diagnosis |
|---|---|---|
| 1 | Berlin blue staining, Gomori, HE (hematoxylin and eosin staining), Masson, CK AE1/AE3, CK7, CK18, D2-40, F-VIII, CD31, CD34 | “piecemeal” necrosis, focal necrosis, bridging fibrosis; chronic active hepatitis |
| 2 | Gomori, HE, Masson | “piecemeal” necrosis, bridging fibrosis; chronic active hepatitis |
| 3 | HE, I.O., CK7, D2-40, F-VIII, CD31, CD34 | Epithelioid haemangioendothelioma |
| 4 | HE, I.O. | Mild surgical hepatitis |
I.O., intraoperative.
Six months later, follow-up contrast-enhanced MSCT of the upper abdomen was performed to evaluate the size of the tumours. Reduced volume of inhomogeneous left liver lobe, with signs of diffuse liver lesion was seen, and caudate lobe hypertrophy was detected. Liver focal lesions were typically with central hypodensity and peripheral contrast enhancement in arterial and portal-venous phase, measuring 43 mm × 43 mm, 22 mm × 16 mm, and 22 mm× 21 mm. No other abnormality was seen in the abdomen or pelvis. Follow up contrast-enhanced MSCT of the upper abdomen 6 months later revealed no further progression in size and number of liver lesions.Laboratory findings revealed normal bilirubin, gamma-glutamyl transferase (GGT) and alkaline phosphatase (ALP), and mild increase of alanine aminotransferase (ALT) (69 U/L, reference range, 9–59 U/L) and aspartate aminotransferase (AST) (62 U/L, reference range, 11–34 U/L).
After a pre-transplantation evaluation protocol, no contraindications for orthotopic liver transplantation (OLT) were revealed, and the transplantation was done in March 2018. Nine months after the OLT the patient was well, with normal liver function and morphology, and without any signs of tumour recurrence.
Discussion
Due to its physiology and histological structure, the liver is potentially affected by a number of primary and secondary neoplasms, the latter being more frequent. Primary liver neoplasms include hepatocellular, biliary, mesenchymal and vascular tumors (5). The most frequent vascular liver tumor is cavernous haemangioma, the benign neoplasm which is a common incidental finding on routine ultrasound examinations of the liver. Primary angiosarcoma is a rare but extremely aggressive (6), while EHL is a rare vascular tumour. The tumour has variable biology, ranged from benign haemangioma to highly malignant angiosarcoma, therefore it is difficult to prognose the outcome. It most frequently originates from liver and lungs. The growth of the tumour is slow, but it can invade the adjacent organs and metastasize (7). The range of the clinical features of EHL varies from completely asymptomatic to liver failure (4). The most common patient complaints include right upper epigastric pain, weight loss and palpable liver enlargement (4).
Laboratory findings may reveal minimal abnormalities in bilirubin, GGT, ALP and ALT, and these findings are completely non-specific (4).
In most cases (>80%), including ours, EHL is a multifocal process, and the solitary focus is far less commonly detected (8). It is not uncommon that this kind of hepatic neoplasm is detected incidentally, during ultrasound, computed tomography (CT), MR, positron emission tomography (PET)-CT or some other tomographic imaging modality performed for reasons other than liver pathology. The findings typically include multiple foci mostly at the periphery of the liver, possibly with retraction of the liver surface. Typical signs are focal liver lesions with hypodense center and contrast-enhancing periphery. In some tumors, fine calcifications may appear. MR and CT appearance are similar as in other hypervascular liver tumours, with ring-like postcontrast enhancement of peripheral viable tumour tissue, and non-enhancing mostly fibrotic or even necrotic central area (9,10). Since EHL may mimic other neoplasms, and can also be diffuse in nature, percutaneous biopsy pathohistological diagnosis (PHD) is an imperative. Diffuse EHL initially presents with several nodules, which grow up and merge during the progression of the disease, finally overwhelming the entire liver (4,7). Typical histochemical feature of EHL is the positivity for CD34 and CD31. Nuclear expression of CAMTA1 is seen in 85–90% of patients, and is critical in diagnosis of the entity (11,12).
Many treatment options are available, including surgical resection, OLT, hormonal therapy, chemotherapy, radiotherapy, transcatheteric arterial embolisation, percutaneous ethanol injections ablation, thermoablation, antiangiogenic agents and watchful observation (4). The most commonly used treatment option is OLT, with its 5-year survival rate of 80% (13). Oncologic treatment remains a solution for inoperable patients (14). Taking into account the expression of vascular endothelial growth factor (VEGF), targeted therapy is based on anti-VEGF agents: bevacizumab monotherapy or in combination with cytostatic agents (capecitabin) is used (15). If the tumour remains unchanged for years, observation can be a satisfactory option (4).
Conclusions
In this case report, we presented a case of rare liver hemangioendothelioma. MR and MSCT revealed multiple focal liver lesions, while ultrasound-confirmed biopsy made the final diagnosis. Due to tumor progression, orthotopic LT was performed as the method of choice. Follow up after one year, done with MSCT and MR, showed no transplant dysfunction and tumor relapse. MSCT and MR are useful in detecting and evaluating the progression of hemangioendothelioma and are excellent radiological follow up methods after transplantation.
Acknowledgments
We highly appreciate the expertise and help of Professor Zoran Brnić, MD, PhD (Department of Diagnostic and Interventional Radiology, Sestre milosrdnice University Hospital Center, Zagreb, Croatia) for critical reviews of the manuscript.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2019.08.06). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer 1982;50:970-81. [Crossref] [PubMed]
- Treska V, Daum O, Svajdler M, et al. Hepatic Epithelioid Hemangioendothelioma - a Rare Tumor and Diagnostic Dilemma. In Vivo 2017;31:763-7. [Crossref] [PubMed]
- Ishak KG, Sesterhenn IA, Goodman ZD, et al. Epithelioid hemangioendothelioma of the liver: a clinicopathologic and follow-up study of 32 cases. Hum Pathol 1984;15:839-52. [Crossref] [PubMed]
- Mehrabi A, Kashfi A, Fonouni H, et al. Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer 2006;107:2108-21. [Crossref] [PubMed]
- Boyer TD, Manns MP, Sanyal AJ. Zakim and Boyer's Hepatology: A Textbook of Liver Disease. 6th edition. Philadelphia: Saunders, 2011. Str. 195-7, 1045-50.
- Bioulac-Sage P, Laumonier H, Laurent C, et al. Benign and malignant vascular tumors of the liver in adults. Semin Liver Dis 2008;28:302-14. [Crossref] [PubMed]
- Requena L, Kutzner H. Hemangioendothelioma. Semin Diagn Pathol 2013;30:29-44. [Crossref] [PubMed]
- Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer 1999;85:562-82. [Crossref] [PubMed]
- Thin LW, Wong DD, De Boer BW, et al. Hepatic epithelioid haemangioendothelioma: challenges in diagnosis and management. Intern Med J 2010;40:710-5. [Crossref] [PubMed]
- Mehrabi A, Hoffmann K, Weiss KH, et al. Long term follow up after resection emphasizes the role of surgery in Primary Hepatic Epithelioid Hemangioendothelioma. Ann Med Surg (Lond) 2016;11:1-4. [Crossref] [PubMed]
- Doyle LA, Fletcher CD, Hornick JL. Nuclear Expression of CAMTA1 Distinguishes Epithelioid Hemangioendothelioma From Histologic Mimics. Am J Surg Pathol 2016;40:94-102. [Crossref] [PubMed]
- Shibuya R, Matsuyama A, Shiba E, et al. CAMTA1 is a useful immunohistochemical marker for diagnosing epithelioid haemangioendothelioma. Histopathology 2015;67:827-35. [Crossref] [PubMed]
- Nudo CG, Yoshida EM, Bain VG, et al. Liver transplantation for hepatic epithelioid hemangioendothelioma: the Canadian multicentre experience. Can J Gastroenterol 2008;22:821-4. [Crossref] [PubMed]
- Thomas RM, Aloia TA, Truty MJ, et al. Treatment sequencing strategy for hepatic epithelioid haemangioendothelioma. HPB (Oxford) 2014;16:677-85. [Crossref] [PubMed]
- Lau A, Malangone S, Green M, et al. Combination capecitabine and bevacizumab in the treatment of metastatic hepatic epithelioid hemangioendothelioma. Ther Adv Med Oncol 2015;7:229-36. [Crossref] [PubMed]
Cite this article as: Hrabar J, Kavur L, Vidjak V, Hrabar M, Bubić V. Epithelioid hemangioendothelioma of the liver—case report. Dig Med Res 2019;2:24.


